The Week in Review, 15 - 21Feb2021
Georgia COVID-19 Updates
Combined Data
The graph below shows how four of our big metrics for tracking the COVID-19 pandemic are tracking over time. Cases are represented by the blue line and correspond with the left y-axis. All other metrics correspond with the right y-axis. The reason I graph all of these things together is so that we can see the way these things trend together (or differently) over time.
This week we saw cases and hospitalizations continue their decrease. However, whereas cases have decreased 69% from the peak on 10Jan, hospitalizations have seen a much slower and smaller decrease - 36%. It’s a good reminder that as good as the news might be that cases are declining, there are still a lot of people out there with serious cases of COVID-19 and the burden on hospitals remains significant.
ICU admissions were about the same as the previous week. Deaths increased 5% this week compared to the previous week’s total.
Testing
This week we saw a plateau for PCR testing. In total, there were 189,168 PCR tests reported. Of those, 10.2% were positive. Both of these metrics are about the same as the previous week. The test output trend over time can be seen in the graph below, represented by the blue line that corresponds with the left y-axis. The red line represents the test positivity rate over time, and corresponds with the right y-axis. The gray dashed line is the goal line for test positivity.
The percent positive rate has decreased, but we still remain far above the 5% goal line. So we are likely missing a lot of cases, but not as badly as during the height of the winter surge.
The Georgia Department of Public Health began providing antigen test data this week, for total tests performed and how many of them were positive. This week we only have a partial week’s worth of data. Of the antigen tests we know about for this week, 7.8% of them were positive.
However the DPH still does not provide data regarding demographic details for cases identified by the antigen test. Keep that in mind as we go through the demographic data in the following sections. You’re only seeing part of the data. Meanwhile, antigen testing identified 32% of the cases this week.
Cases
The number of combined new cases (by date of report) is as follows:
- 24 hours: 1463 by PCR + 295 by antigen = 1758 (+0.2%)
- 7 days: 14,033 by PCR + 6,735 by antigen = 20,768 (+2.2%)
- 4 weeks: 86,280 by PCR + 32,314 by antigen = 118,594 (+13.7%)
The new statewide total is 985,505, combining PCR and antigen-test identified cases. We will likely cross 1 million cases this week. Bear in mind that because our test positivity rate is so high, these numbers are likely an under count of the disease burden. In the graph below, I show the Georgia cases by date of report for both PCR and antigen cases for each county type. Ignore the big bump around 11Oct - that was a data dump of antigen cases. You can check how your county is classified here. The state’s case rate is now 18% below the peak of the summer surge, but 176% higher than the pre-winter surge baseline. We likely have at least one more surge to go before enough people are vaccinated to start our steady march down for good. We need to get back to that baseline or the next surge will have the momentum to peak even higher than the winter surge.
The next two graphs show us some of the demographic details of those who are getting sick and testing positive. In each graph, you’re looking at 8-week timelines for each age group side by side.
This week we saw decreases in cases for every age group However, cases are still quite high. A really good thing we see in this graph is a negative number in the “unknown” category. This is a holding spot for cases that are pending investigation and follow up. When the numbers are large for this category, it suggests that contact tracers are overwhelmed by the number of cases. When the number is small, it suggests they’re coping. When the number is negative as it is this week, it suggests that contact tracers are not only able to cope with the week’s incoming cases, but can work through the backlog that preceded this week.
The steep decline we’re seeing in cases for Georgia is likely not due to the vaccination effort - not yet anyway. It has to do with the population of people we’re targeting for vaccination. The goal the Governor has put forth has been to prevent deaths. As you’ll see in later graphs, the majority of our deaths come from those 70+. So in addition to healthcare workers, the state has targeted these seniors in the early vaccine eligibility phase. If the goal was to prevent transmission (or decrease cases) then we would need to target a different age group - those 18 - 59 - because they contribute the majority of our cases. The earliest place we should see the impact of the vaccines should be deaths primarily, but also hospitalizations. We aren’t yet seeing a decrease in deaths. However, death reporting is even more delayed than case reporting. So it’s possible that we are actually experiencing a decrease that we just can’t see in the data yet.
Hospitalizations
The number of combined new hospital admissions (by date of report) is as follows:
- 24 hours: 106 new COVID-19 admissions, 3 admissions to the ICU (weekend reporting is typically light)
- 7 days: 1374 new COVID-19 admissions, 167 ICU admissions
- 4 weeks: 6368 new COVID-19 admissions, 728 ICU admissions
According to the state of Georgia, the number of patients currently hospitalized for COVID-19 is 2353 and we haven’t been been at a level this low since 3Dec. According to the US Department of Health and Human Services, they’re tracking that Georgia currently has 2865 patients hospitalized for COVID-19. The discrepancy is likely due to the fact that HHS includes suspected COVID-19 case admissions and pediatric admissions whereas the state of Georgia does not report either of those populations in their number. According to HHS, there are 47 children currently hospitalized for COVID-19 in Georgia.
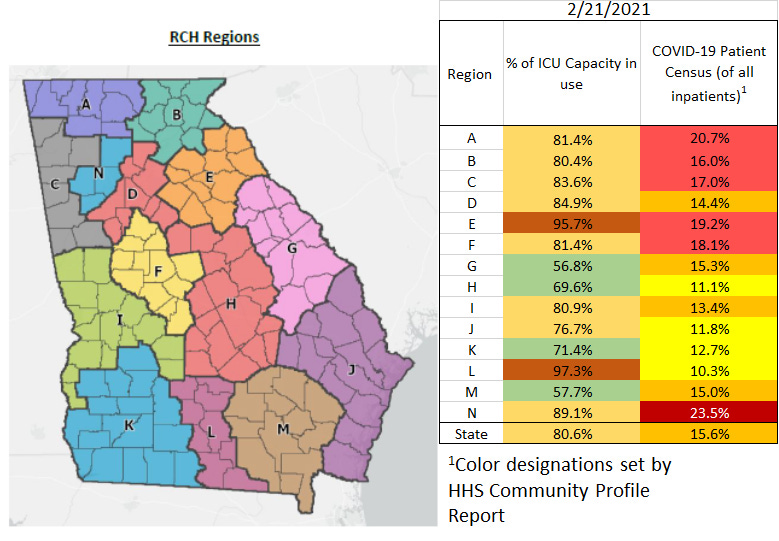
The graphic below shows us the Georgia Emergency Management Agency hospital regions. The table on the right tells you how each region is doing with respect to usage of their available ICU beds and how their COVID-19 patient population compares to their overall patient population. These numbers are all based on data from the Georgia GIO COVID-19 data hub.
There’s a LOT of news to celebrate here. There are now just two regions using >90% of their ICU beds (E and L). And for region N (NW Atlanta suburbs), this is the first time they’ve been using less than 90% of their ICU beds since 15Nov. In addition, if we look at the patient census, the state is now in the orange zone as are 4 regions. There are four regions in the yellow zone. As recently as 18Jan, all regions were in the dark red zone. Regions H, I, L and M have reached their pre-surge baseline.
The state says that 80.6% of ICU beds are full whereas HHS says the number is 84%. I’ve started to graph both numbers, with the HHS estimate in orange below. The HHS reports that 29% of the ICU beds in Georgia are occupied by COVID-19 patients. This is a big improvement compared to the height of the winter surge, when more than half of ICU beds were in use by COVID-19 patients.
As a reminder, hospitalizations are down - yes. But they aren’t dropping as fast as cases and remain at a high level. We see a lot of improvement for regions of the state but the state still has the highest confirmed COVID-19 admission rate in the country, tied with Kentucky. We need to continue to do the long, difficult work of limiting disease transmission to give our healthcare workers the space they need to do their jobs well and to give them time to recover. We need to bring the entire state back to the pre-winter surge baseline.
Next, let’s look at the demographic details that we have for hospitalizations.
This week hospital admissions increased for infants <1 year old, and 30-39 year olds. They were flat for 10-17 year olds. Hospital admissions decreased for all other age groups. They decreased for all races too (data not shown).
In Georgia, the COVID-19 hospitalization rate, on average, is 5.6%. For those who are hospitalized, 16.3% require an ICU bed. While the case fatality rate for confirmed cases and confirmed deaths right now is 1.77%, the fatality rate for people admitted to the ICU for COVID-19 is 40.4%. The ICU mortality rate has increased 7.6% since I started tracking this information, the week of 10Oct.
Deaths
The number of new confirmed deaths (by date of report) is as follows. The percentage in parentheses indicates how the increase compares to Georgia’s cumulative total at the start of each window of time.
- 24 hours: 4 (+0.03%), -2 probable deaths (probably a data correction by the state)
- 7 days: 669 (+4.8%), 204 probable deaths
- 4 weeks: 2832 (+24%), 662 probable deaths
This week the number of confirmed deaths increased slightly, by 5% compared to the previous week. The graph below shows how the 7-day death rate per 100,000 residents has trended over time for each county type. The state death rate is 35% above the peak during the summer surge. The death rate is worst for rural counties and best for the Atlanta counties of Fulton and DeKalb. In fact, the death rate in rural counties is 84% higher than the death rate in Atlanta.
Next, let’s look at the demographic data for this week’s deaths. Deaths increased for those 50-79. Deaths decreased or remained steady for all other age categories.
If we look at race, deaths are declining for the White population but increasing for people of color. Hopefully this trend reverses in next week’s update.
That’s it for today. I will be back tomorrow to discuss how the state fits into the national and global context.
References
https://dph.georgia.gov/covid-19-daily-status-report
https://covid-gagio.hub.arcgis.com/
https://beta.healthdata.gov/dataset/COVID-19-Community-Profile-Report/gqxm-d9w9
https://healthdata.gov/dataset/covid-19-reported-patient-impact-and-hospital-capacity-state
Georgia COVID-19 Updates is a free newsletter that depends on reader support. If you wish to subscribe please click the link below. There are free and paid options available.
My Ph.D. is in Medical Microbiology and Immunology. I've worked at places like Creighton University, the Centers for Disease Control & Prevention and Mercer University School of Medicine. All thoughts are my professional opinion and should not be considered medical advice.