The Daily Digest, 17Jul2020
Georgia COVID-19 Updates
Good evening! We made it through another week in this pandemic. Just a reminder that the newsletter is going out on Monday, Wednesday, Friday, Sunday as I’m preparing for a cross-country move. On Sunday I’ll be compiling a Week in Review.
One other announcement is that I’m launching a podcast next week on Wednesday, July 22nd, and it is called Public Health for the People. Here’s the link for the teaser on Spotify. Here is the blurb:
When the COVID-19 pandemic began, Dr. Amber Schmidtke realized that there was a gap between the way that public health scientists look at data and how the public could understand it. Pairing her experience in public health at the Centers for Disease Control and Prevention and her skill with educating adult learners in the undergraduate and medical school setting, Dr. Schmidtke excels at making complex data meaningful for non-scientists. In this podcast, Dr. Schmidtke helps the public to understand the latest trends for the COVID-19 pandemic in Georgia and explores broader public health topics to improve public trust and to highlight the heroic but often unrecognized work of public health professionals. Public Health for the People is produced and distributed by Could be Pretty Cool.

Testing
Testing is holding steady and today the Public Health Commissioner and the Governor acknowledged that we don’t have enough testing capacity to meet demand right now. Hopefully that will be improved in the coming weeks. For now, our percent positive rate for testing is 16% today. We want to be at or below 5% to contain the virus. That seems counter-intuitive. Why would we want to spend all of this time, effort and money to run a bunch of negative tests? Well, we want to be testing enough people that we ensure we aren’t missing asymptomatic carriers that could transmit the disease to others.

Cases
Today there were 3908 new cases reported. This is the second highest day we have recorded to date. The new statewide total is 135,183. Below you can see how today’s new cases compare to our history. New cases by date of report are in purple. The 7-day moving average is the red dashed line, allowing us to see the trend through the noise.

Nearly 1200 of today’s new cases came from nonrural counties that aren’t part of the Atlanta metro. An additional 1013 came from the Atlanta Suburbs. Today at Governor Kemp’s news conference he made a claim that isn’t supported by the state’s public health data. The protests in Atlanta following the murder of George Floyd did not trigger a surge in cases in those counties. Those counties are certainly not free of disease, but they are not hot spots. The areas with greatest increase are nonrural counties, especially along the Georgia coast and our border counties - areas affiliated with tourism and hospitality.
Below you can see where cases have been surging most over the past 14 days. The darker the shade, the more intense the increase. The legend is % increase over 14 days.

You can see that the darkest regions are still clustered along the Georgia coast, the South Carolina border, and central Georgia. In the table below you can see counties that are on the counties of concern list for having a >50% increase over the past 14 days. There are 72 counties on the list, plus the non-Georgia resident category, representing 45% of the state’s 159 counties.

One important thing to notice is just how many of these counties are rural, and in fact those counties are some of the areas with greatest increase. Below you can see how cases have accumulated since the beginning of the pandemic, by county type.
Hospitalizations
The most concerning thing, to me, is the situation surrounding hospitalizations. We continue to set records with the number of patients currently hospitalized for COVID-19. Below you can see how this has trended over time. Today’s new record is 2902. As has been the case for the past 17 days, this is a new record since GEMA began providing these data.
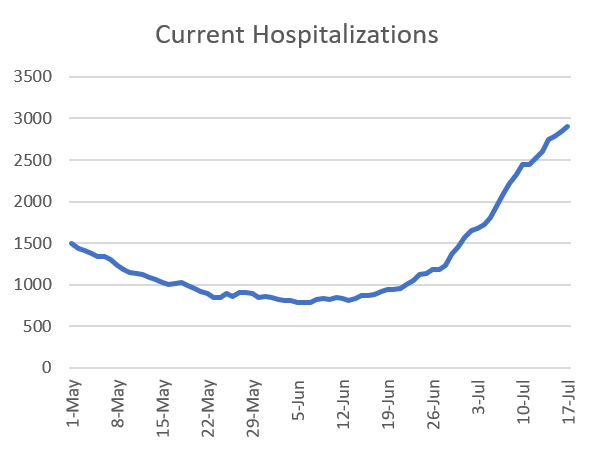
But it’s not just those currently in the hospital that is increasing, but the number of new patients coming into the hospitals - who will add to the current hospitalization rate over the days and weeks to come. The graph below shows how many new hospitalizations have been reported each day (purple) with the 7-day moving average in orange. The trend has been increasing steadily for the past three weeks, increasing the strain on our healthcare infrastructure.

Critical care beds and ventilators are some of the resources of greatest need for the most severe forms of COVID-19. Unfortunately, use of both of these resources has been on the rise too. Below you can see how adult ventilator use has trended over time (blue line) and the 7-day moving average is in orange. It has been trending upward steadily for the past two weeks. At present, GEMA does not provide data on pediatric ventilator availability, something I hope they will remedy before schools reopen.

Below is the second page of the GEMA daily situation report for 17Jul2020 (today). Only 15% of the critical care beds in the state are unoccupied right now. Some will wonder how that compares to historic trends and to that I would argue that it would be interesting to know but not that relevant. We are dealing with a crisis right now with surging cases and hospitalizations and those hospitalizations often require critical care. Knowing that we are adding increasing numbers of new hospitalizations each day, we need to know what resources we have to deal with the problem now. And that resource is under strain.
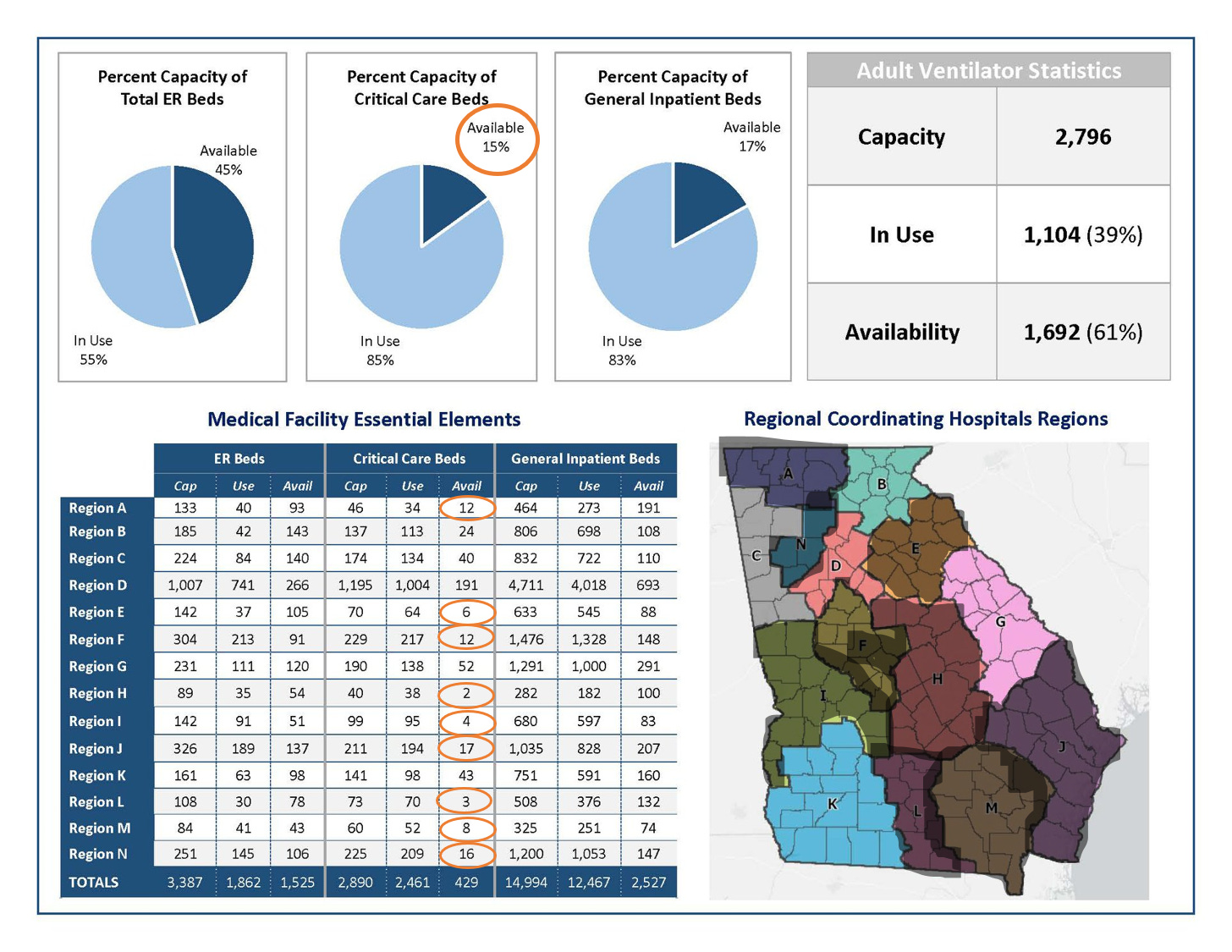
The other thing to notice is in the table on the lower left where it shows the critical care bed capacity by hospital region. Only five of the state’s 14 hospital regions have >20 critical care beds available. I’ve shaded in the hospital regions that have limited or critically limited ICU bed capacity right now. You can see the impact this is having on a person’s ability to access care in a timely fashion if they develop severe COVID-19 complications.
It’s also important to remember that survival and death aren’t the only outcomes of COVID-19, for as many people want to say that we should get back to normal because 98% of people survive. Here’s a study that came from Italy, the previous epicenter of the pandemic. They looked at the symptoms hospitalized patients experienced while they were acutely ill and in the hospital and then the symptoms they were experiencing up to 60 days after discharge. Some key findings:
Only 12.6% were completely symptom free after surviving COVID-19, meaning 87.4% had long term effects.
32% had 1-2 symptoms
55% had 3-4 symptoms
44% had worsened quality of life 60 days after discharge
Below you can see the symptoms patients experienced both acutely and long term. There are some words in here you may not be familiar with. Dyspnea = shortness of breath. Anosmia = lost sense of smell. Sicca syndrome = related to an autoimmune disorder, but dry membranes of the eye and mouth. Rhinitis = runny nose. Dysgeusia = altered sense of taste. Myalgia = muscle pain.

This is a small sample size and only looks at hospitalized patients, rather than those who managed their care at home. But still, it seems a bit disingenuous to assume that people are going to get this and it’s going to be like a flu or cold. It is not a benign infection that people get over and are as good as new afterwards. We don’t have enough time to know the long term impacts of this disease yet. You can listen to one man’s experience surviving COVID-19 on my friend Rev. Jake Hall’s radio show, Gospel Gothic.
Deaths
There were 28 deaths newly reported today, a low-medium day for us. The new statewide total is 3132. Twelve of today’s deaths came from nonrural counties, with 5 coming from Troup county, alone.
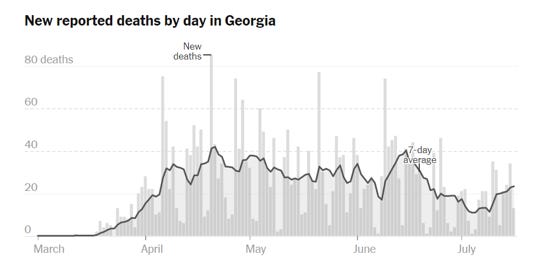
Below is the New York Times’ graph of Georgia COVID-19 deaths by date of report. The dark line is the 7-day moving average. What you can see is that we’ve had an increase over the past week or so. This could be noise, or it could be the beginning of a larger increase that was predicted to follow the surge in cases and hospitalizations. We need more time to know for sure.
The last graph today shows how cases and deaths have accumulated over time, since the beginning of the pandemic. Cases are graphed using the left y-axis. Deaths are graphed using the right y-axis. Keep in mind these are not on the same scale. There are not more deaths than cases, for example. But it allows us to see the trends for both things at the same time.

We see that cases took a sharp turn upward starting around 17Jun, and we have what looks like exponential growth (scary words for anyone who works in public health). We also see that deaths have had a steady increase that leveled around 17Jun but started to rise more significantly around 01July. What I worry about is whether that red line is going to swing sharply upward like the case curve.
So please do all that you can to minimize your exposures. Avoid unnecessary errands and travel. Keep a distance of 6 feet when near people who don’t live with you. If social distancing cannot be maintained, then wear a mask. Avoid indoor gatherings as much as possible. Keep washing your hands regularly and observe excellent sneeze and cough etiquette.
I’ll see you on Sunday. Be safe and be well!
References
https://dph.georgia.gov/covid-19-daily-status-report
https://www.facebook.com/GEMA.OHS
https://jamanetwork.com/journals/jama/fullarticle/2768351
https://www.mixcloud.com/thecreekfm/gospel-gothic-ministers-lament/
https://www.nytimes.com/interactive/2020/us/georgia-coronavirus-cases.html

Thank you so much for taking the time to share these updates! It’s so hard for a lay person (such as myself) to find reliable data and correctly interpret it and I just wanted to say I appreciate you so much. 🙂
Thank you for these updates. You mentioned Georgia hospitalization stabilizing. Arizona appears to be going down. Obviously this could be from social behavior mask ect. There was a New York times article about Arizona with zero mention that the virus could be slowing because there are more immune people out there. You didn't mention it either as a possibility in Georgia stabilizing. That seems the most obvious and it is really early to know but it seems it's worth a mention. I took one semester of Virology and you have a PhD so what am I missing?. Is this just not a possibility or are the experts afraid to even raise the point until they are absolutely sure out of fear that people will let their guard down?