Good afternoon! I’m sure you’ve heard the news reports, but things are getting intense in other parts of the country. In fact, the state where I live now (Kansas) has tipped over into exponential growth of cases, similar to what we experienced in the summer. We aren’t seeing that exponential growth in Georgia yet. But we should do all that we can to prevent that from happening. In the absence of government intervention, we are largely dependent on the collective action of individuals to follow the public health guidance that we’ve had this whole time. The guidance may be cumbersome or uncomfortable, but it works. We just need more people to follow it. Thank you for doing all that you can to limit disease transmission.
And if I haven’t said it in a while, I just want to send a message of respect and support to anyone who follows this newsletter who works in public health or who is a healthcare worker. I imagine you are so weary and tired. Thank you for all that you are doing and I hope you know how important you are. We owe you so much.
Testing
Today there were 31,137 new PCR tests reported, and this is a high number for us, especially in the past month. Of the new PCR tests reported today, 7.4% were positive. One hundred percent of these tests were reported through ELR, so today’s positive rate is as solid of an estimate as it gets. Of the cases that were identified through PCR and reported today, only 10.6% were backdated prior to the 14 day window of uncertainty. So the cases identified today are recent and/or current, at least for the cases identified by PCR. We have no supporting data for the cases identified through antigen testing. Given how quickly they turn around a result, it stands to reason that they are mostly current/recent. But we had a data dump earlier this week of about 1000 results that were from mid-October. So antigen cases aren’t immune to this problem of delayed reporting. They still count, of course, they just aren’t recent or active cases.
Cases
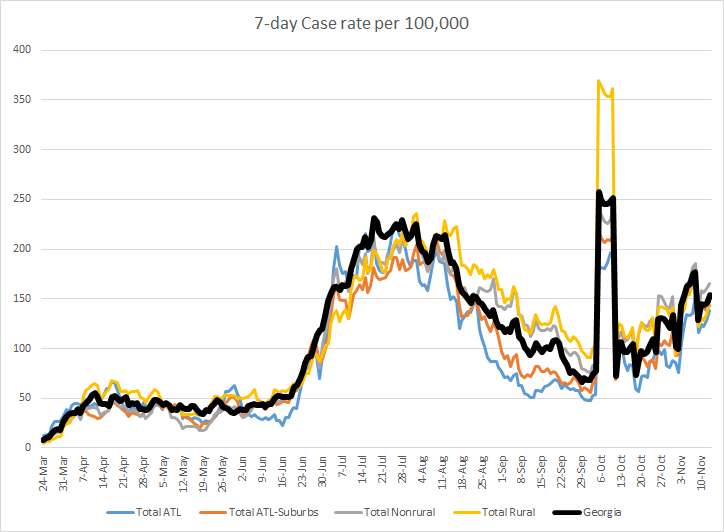
There was a net increase of 2994 cases reported today and 23% were antigen cases. The new statewide total is 419,870 with 382,505 identified by PCR test and 37,365 identified by antigen test. For today’s cases, 33% came from nonrural counties outside of the Atlanta metro, 26% came from rural counties, 21% came from the Atlanta suburbs. If you’d like to check your county’s classification, this post might be helpful. In the graph below, you can see how things are trending over time across different county types. Ignore the big spike around 06Oct - that’s when DPH first told us about the antigen cases (~26,000 up to that point). Pay attention to the trend after it.
I wanted to take a closer look at Whitfield county in northwest Georgia today, with one of the highest 2 week case rates in the state. If we look at their case graph by date of symptom onset, we see that their 7-day average is about 30% less than their peak during the summer. There are some big days in the 14-day window for Whitfield county too. So there are some concerning increases in Whitfield county.
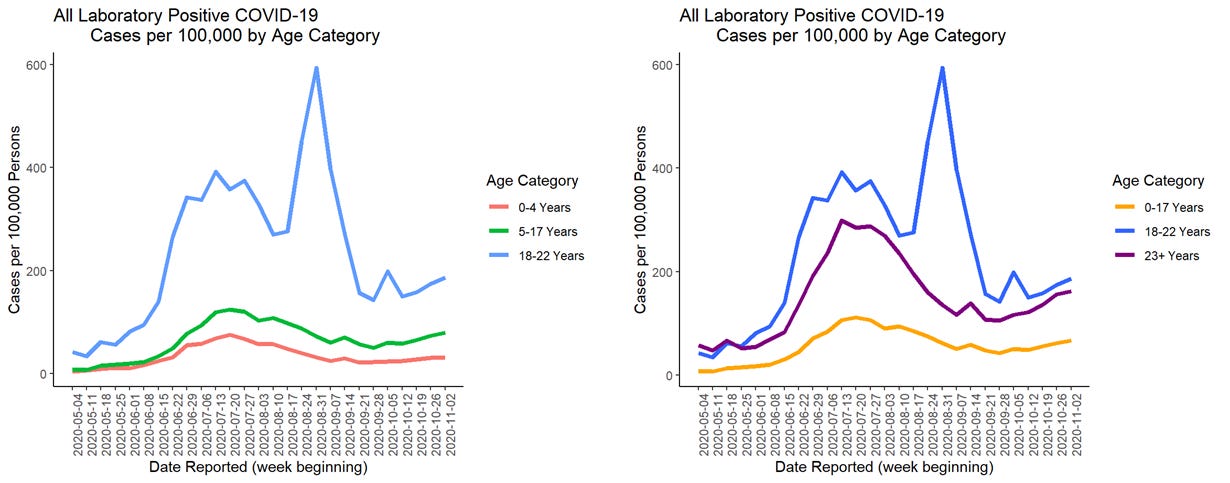
In this week’s School Aged Surveillance Data Report from DPH, we now get the inclusion of antigen test-identified cases. The left graph shows younger populations. The red line corresponds to kids 0-4, the green line represents K-12 aged children and the blue line represents college aged adults. The graph on the right shows the entire Georgia population’s cases. The pediatric cases are represented by the yellow line, college aged adults are the blue line and everyone older than 23 is represented in the purple line.
The big thing to take away from this graph today, I think, is that cases are increasing for every age group.
The most recent week saw fewer school-based clusters of illness (a good thing). We don’t get any additional data regarding how many cases, hospitalizations or deaths are associated with each cluster. Remember, the DPH does not distinguish K-12 versus college or university. They’re all counted as “schools.”
Hospitalizations
There were 142 patients newly hospitalized for COVID-19 today and 20 newly admitted to the ICU. Twenty-eight percent of adult ventilators are in use as of today and that is consistent with the levels that were typical before the summer surge. As of today, there are 1686 patients currently hospitalized for COVID-19 and we are trending up (see below).
In the summer we saw exponential growth of the currently hospitalized population. We don’t want to see that again. The problem with exponential growth (among many ugly consequences) is that we don’t recognize that it has begun in real time. Everything looks okay (or not so bad) until it’s not and then it’s really not okay. It can overwhelm hospitals when this happens, as we’re seeing elsewhere in the country. Often, by the time we realize there’s a problem, even if we locked everything down completely (which I think is unlikely anyway) then we wouldn’t see an impact for 2-3 weeks. That’s because the people who are going to be sick next week were exposed this week. The people who are going to be admitted next week were exposed 1-2 weeks prior. We get to control how big the next hospitalization surge becomes with our actions. You avoid hospitalizations by avoiding cases. If we can limit how many people get infected, the virus has fewer opportunities to harm our population.
Deaths
There was a net increase of 15 confirmed COVID-19 deaths reported today, a mercifully small number after the last two days of 69 and 70 deaths. The updated total is 8418. Here is the updated death rate graph over time, comparing the rates across different county types in Georgia.
Deaths are trending up again, but this could be some of the same noise we’ve seen before (i.e. see what looked like an increase starting 17Sep). The state average is trending up and that is driven by increases in all county types other than nonrural counties. The 7-day death rate in rural counties is 74% higher than the state average.
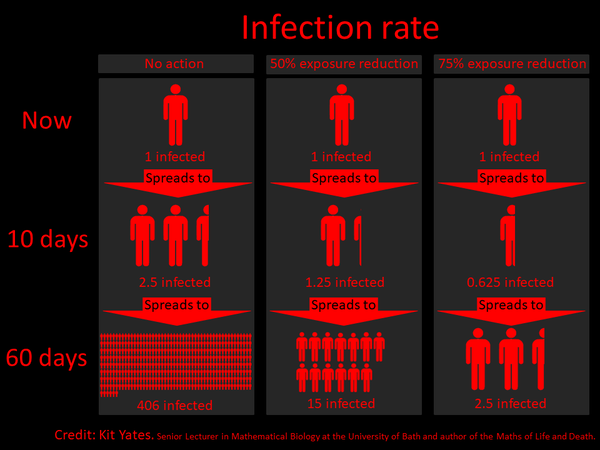
I saw this graphic on Twitter recently and thought it was helpful for us to visualize how our seemingly innocuous encounters, say at the grocery store or church or at a party, don’t hurt people in the short term, but can in the long run if we aren’t careful. The column on the left might represent the person who thinks this whole thing is a hoax and eschews wearing a mask, social distancing, etc. And if they’re unknowingly infected, they will on average infect 2.5 other people over the next 10 days. Then each of those people will go on to infect an additional 2.5 people. It grows to as much as 406 infected people within 60 days, just from brushing shoulders with someone while unmasked in the cereal aisle.
Let’s say that you wear a mask (A good thing! Go you!) but maybe you had some close encounters indoors. Or you met inside for an hour while socially distant, but no one was wearing a mask. You might fit into the middle column. You were using a prevention strategy, but no one strategy is perfect. So you’ve reduced your exposure risk by 50%. That means that if you’re unknowingly infected, you go on to infect 1.25 people. In the coming months, that 1.25 person goes on to infect another 1.25 person, etc. In 60 days, it can amount to as many as 15 infected individuals. There’s a huge benefit to this, with 96% fewer people getting sick, even though some folks do still get sick. Please employ at least one strategy for avoiding disease at all times.
Let’s say that you are wear a mask regularly and are a stickler for social distancing (way to go!!!). But maybe there was a slip somewhere along the way and now you’re infected (maybe asymptomatically). Because of how careful you are, you only infect less than one person. That person may or may not go on to infect other people and at the end of 60 days, only 2.5 people in total are infected.
So you see, the power to stop this pandemic begins with each of us. We can reduce infections by 96% by using at least one strategy for avoiding illness (I strongly suggest that wearing a mask be your go-to). If we do more than one prevention strategy, then the spread becomes virtually non-existent. We have widespread, uncontrolled community transmission - both in Georgia and across the United States. We are more of the left column than the middle or right column. We need for people to realize that this is real and just because someone doesn’t drop dead in front of you because you bumped into them (while unmasked) while grabbing a can of soup does not mean they won’t in the coming weeks from that encounter. I think a big problem with this pandemic is that people don’t see the consequences of their actions (or inactions) in real time. It gives a false sense of security that “nothing happened” and we can continue to go to a bar or to the gym or eat in a restaurant with friends. We don’t get to see what happened to the people who were running on the next treadmill over or dining at the next booth.
So remember, we have the power to control how high this next surge goes. Even if we can employ one preventative strategy - such as wearing a mask - we reduce the number of cases by 96%. We could be done with this ongoing rollercoaster of disease surges if we could get better adherence to public health guidance. I guess this is just my frustration bubbling over. I haven’t eaten in a restaurant since mid-March. I miss going to the movies. I want more than anything to see my extended family for Thanksgiving. I know for many of my readers, I’m preaching to the choir. Thank you for all that you are doing. Maybe this will be the message that matters to one new person.
Be safe and be well! Talk to you again on Sunday.
References
https://dph.georgia.gov/covid-19-daily-status-report
https://covid-gagio.hub.arcgis.com/
https://amberschmidtkephd.substack.com/p/pcr-percent-positive-rate-by-county
https://epidemiologyschoolreport.s3.amazonaws.com/SchoolAgeSurveillance1102.html#statewide-data
Georgia COVID-19 Updates is a free newsletter that depends on reader support. If you wish to subscribe please click the link below. There are free and paid options available.
My Ph.D. is in Medical Microbiology and Immunology. I've worked at places like Creighton University, the Centers for Disease Control & Prevention and Mercer University School of Medicine. All thoughts are my professional opinion and should not be considered medical advice.