This is obviously an historic and deeply unsettling day. I honestly debated whether to even write today, considering what is happening in Washington, DC. I just want to reach out through the email and internet to say that if you’re having a hard time with this, on top of everything with COVID, feel free to skip this email. It will be okay. We will be okay. Take care of yourself, for now, if that’s what you need.
The DPH came out with an announcement this afternoon that their data would be delayed due to a high volume of data to process. We’re well past the estimated time that they thought the numbers would go up. So this seems ominous. In the meantime, we do have other things to discuss.
Vaccine Update
According to the CDC’s COVID Vaccine Tracker, 4,836,469 Americans have initiated their 2-dose COVID-19 vaccine series.
I know there are legitimate concerns about safety with the new COVID-19 vaccines. The clinical studies showed that the most common side effects were similar to what you see with the flu vaccine, things like pain at the injection site, fever, fatigue, headache, etc. Many of these things are signs of inflammation - your immune system is responding to something new - exactly what we want your immune system to do with a vaccine. But as the vaccine studies looked at tens of thousands of people. As the vaccine is used more widely in the population, any adverse events are reported through the Vaccine Adverse Event Reporting System. The data are available to the public. A couple reminders, these events are reported and pending investigation to determine whether the adverse event was due to the vaccine or an unrelated cause. But it’s an early look at things.
I sorted the search criteria to limit it to events considered serious and associated with an emergency room visit. So far there have been 29 people that fit these criteria and the top symptoms experienced are listed below. There are 278 symptoms listed. Just keep in mind that people can experience more than one symptom at once. Some of the “symptoms” are laboratory results, including normal findings - see the row below that says “blood magnesium normal.” Also, some of the symptoms are redundant depending on how the report was submitted. For example, tachycardia means elevated heart rate. But if the person submitting the report said “heart rate increased” as in the last row below, then that’s a separate symptom listed even though they’re the same thing. So these things explain why there’s a disagreement between 29 and 278. A lot of these medical terms will be unfamiliar. Dyspnoea = shortness of breath, Tachycardia = rapid heart rate, Paraesthesia = altered sensation (i.e. pins and needles), Angioedema = painless swelling under the skin associated with allergic reaction, Dysphagia = difficulty swallowing, Dysphonia = difficulty speaking.
So, there have been 29 people with serious events associated with an ER visit out of 4.8+ million people who have started the vaccine series (or 0.000006%). And not all of those will ultimately be determined to be associated with the vaccine. But even if all of these were definitively linked to the vaccine, the vaccine still seems to be very, very safe for the larger population so far. That’s reassuring news, and I’ll be sure to keep an eye on this to let you know if there are big deviations.
Important caveat: the VAERS system is updated every Friday, so the total numbers (29 people with serious events needing an ER versus 4.8+ million people starting the vaccine series) is asynchronous. Going forward, I’ll note both numbers on Fridays. And both data collection streams might be susceptible to delayed reporting.
The vaccine roll out has had sort of a “the buck stops with no one” theme. Instead of 1 national strategy or 50 state strategies, the responsibility has been passed to local health districts, so that there are thousands of public health district strategies across the nation to immunize the nation. Georgia has 18 different public health districts, that are all understaffed, underfunded, and weary from managing the tasks of also shouldering the responsibilities of testing, cluster investigation, contact tracing, etc. Pushing the vaccine roll out onto them at this stage seems unfair and doomed to fail. This needs to be a team effort, using all the resources at the state or nation’s disposal - including the National Guard, FEMA and state emergency management agencies, etc. We need to start hearing more ideas rather than excuses from leadership at all levels. The new US Congress was just sworn in, the Georgia legislative session will begin this month. This is the time to lean hard on your elected representatives via phone, email, etc, to prioritize more money and effort toward vaccination and public health overall. In the meantime, each of Georgia’s 18 public health districts are trying to organize their own appointment system for scheduling COVID-19 vaccinations. You can look up your public health district and then keep an eye out for those vaccination appointment systems through their websites or social media pages. I was really hoping for a centralized, state-level appointment system, but it seems that it isn’t coming.
Today we will discuss the most recent White House Coronavirus Task Force Report for Georgia. Some of the most notable statements in the summary and recommendations page include:
Georgia has seen high new cases despite a significant decline in testing, an increase in test positivity, and rapidly rising COVID hospital admissions. All are consistent with a full pandemic resurgence.
97% of the state’s counties have moderate to high levels of community transmission.
Significant continued deterioration, from California across the Sunbelt and up the east coast, despite low testing rates during the holidays, suggests aggressive community spread.
They speculate that the acceleration of the fall/winter surge compared to the spring and summer surges might suggest that there is a USA variant of the virus that evolved here, in addition to the UK variant that is more transmissible. Aggressive mitigation must be used in response to a more aggressive virus.
They recommend an “all hands on deck” effort to get the vaccine out, including using nursing students.
They talk about the importance of transparent vaccination strategy and implementation and using dashboards to improve public understanding and trust in the effort. They specifically cite the dashboards of Nebraska and Michigan as examples of best practices. Side note: I would love to see this for Georgia, but it sounds like we’re out of money for just about everything. So big thanks (sarcasm) to the WHCTF for telling Georgia to do this, but not providing any money to do so.
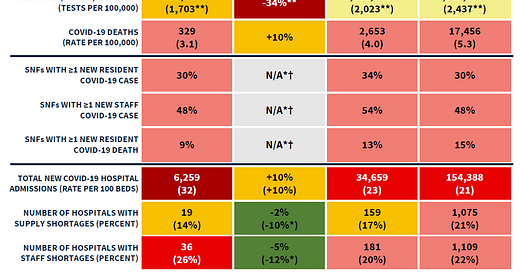
Here’s the summary table from the report. You can read the report in full here. Georgia is ranked #9 for new cases per 100,000, #8 for test positivity, #5 for new hospital admissions per 100 beds, and #44 for new deaths per 100,000.
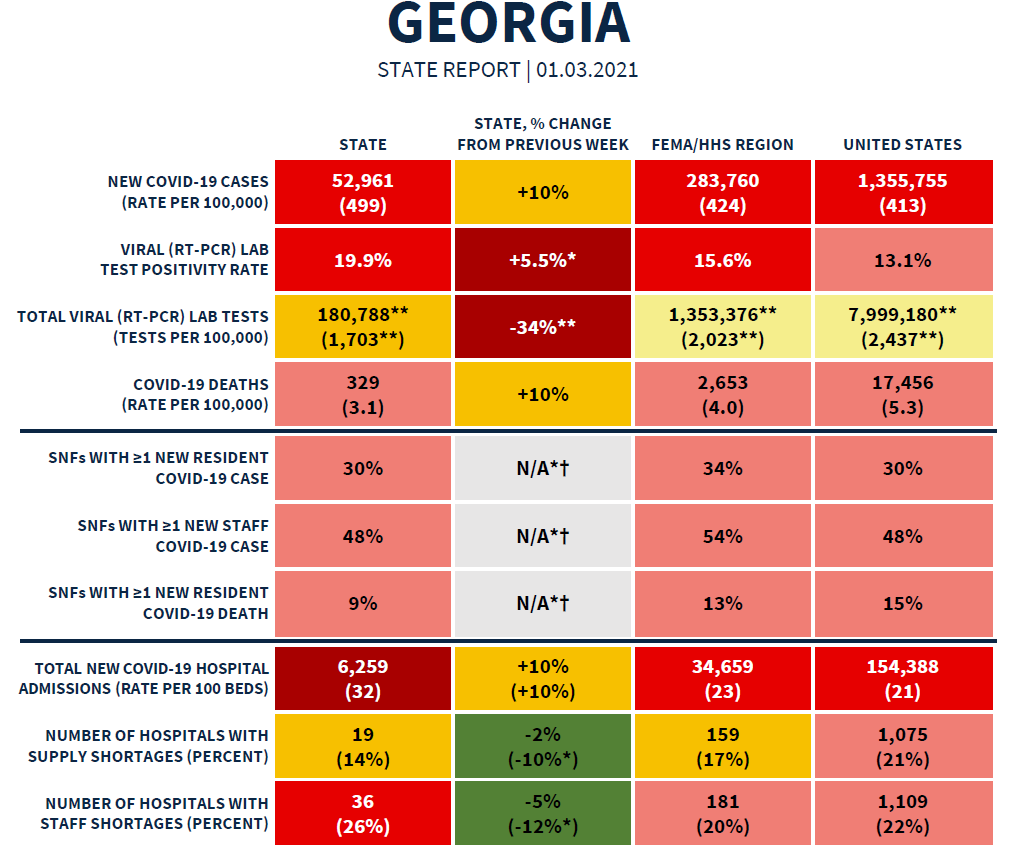
Testing
We’ve seen a national and state-level decline in total test output following the holidays (left graph below). Georgia remains below the national average for testing its population for COVID-19. Meanwhile, test positivity (right graph) has risen for both the nation and the state, but more dramatically for Georgia. We’ve been above the national average for test positivity since early December. One in five COVID-19 tests was positive in Georgia last week. Keep in mind, these reports don’t consider antigen test data.
Cases
The map on the right shows the new case rate per 100,000 for each county in the US. You can see that most of the country is shaded in red. The case rate per 100,000 over time for Georgia (blue line) and the nation is graphed on the left. We remain above the national average for new case rate and we are climbing.
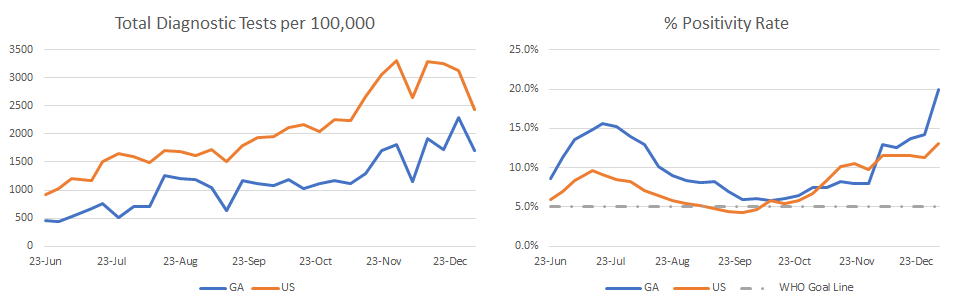
Hospitalizations
The left side of the graphic below comes from the WHCTF reports. The right side of the graphic uses data from the HHS Community Profile Reports. Starting with the graph on the upper left, the COVID-admission rate for Georgia is climbing quickly. The state’s admission rate is 52% higher than the national rate. The map in the lower left shows us where COVID-19 hospital admissions are most intense. Unfortunately, it is intense throughout several regions of the state.
Moving on to the right side of the graphic, the graphs show us how Georgia is doing relative to the nation when it comes to the COVID-19 burden on ICU beds and ventilators. We’ve only had data on this since December 20th, so we don’t have as much historical context as for the other data. But we can see that Georgia is experiencing a greater burden than the national average and the gap is widening.
According to the WHCTF report, Georgia is below the national average for hospitals reporting a supply shortage (14% versus 21%) but above the national average for hospitals with staff shortages (26% versus 22%). These staff shortages are due, in part, to staff getting sick or being quarantined due to COVID-19 exposure.
Healthcare workers have been working under incredible strain for almost a year. They plead for government and community action to save lives and alleviate their burdens, so that they can better care for those who are ill. And they are met with conspiracy theories and people who seek to minimize the importance of the disease. They are met by people who tell them to “suck it up and deal” as they suffer from burnout and PTSD. We are pushing our healthcare workers to the breaking point, logistically and mentally. In California, Los Angeles county has issued guidance to emergency medical service personnel that they should not transport people to the hospital who have a low chance of survival, due to crowding in the hospitals and a shortage of oxygen. Imagine being that ambulance crew, with a scared and worried patient and their family, having to quickly calculate that person’s odds of survival and then tell them that you can’t take them to the hospital. We will be lucky if we don’t see a mass exodus of healthcare workers from the healthcare field after sustaining these moral injuries. We already have a substantial nursing shortage in this country. It takes a minimum of ten years to train a physician. When we lose these people, it will take a long time to replace them. We have to heed their warnings that things are as bad as they say. We see it in the data too.
Again, DPH numbers aren’t published for today. But here’s what we know from the Georgia Geospatial Information Office data hub for COVID-19 regarding hospital usage.
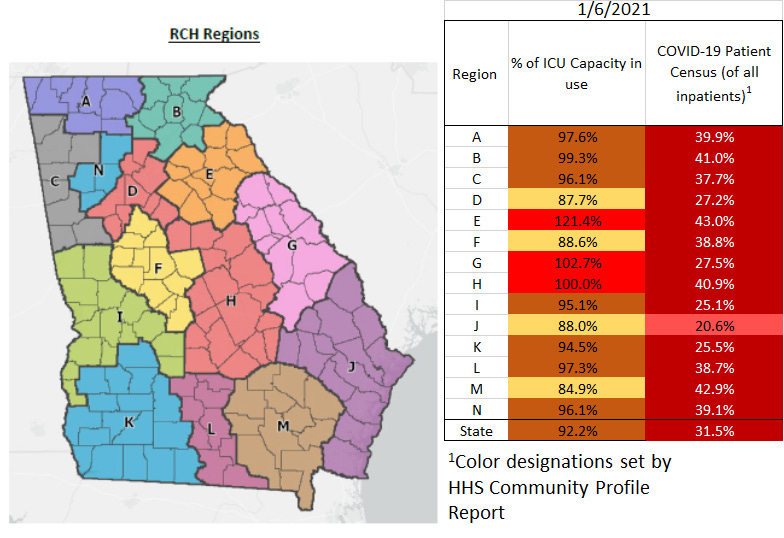
There are three hospital regions that are maxed out for ICU bed usage, regions E (121%!!!), G and H. Ten of the fourteen hospital regions are using >90% of their ICU beds.
Next, let’s look at data from the HHS Community Profile report for 05Jan2021. I’ve copied part of the spreadsheet here for hospital utilization and sorted by the second column (confirmed COVID-19 admissions per 100 beds - last 7 days). Georgia is still ranked #1, alongside Oklahoma. Our neighbors Alabama and South Carolina are also in the top 10. This chart also helps us to see that 44% of the state’s ICU beds are occupied by a COVID-19 patient (8th column) and COVID patients are using 15% of the ventilators too. We are not the highest state for these last two metrics - demand is even more intense in California, Alabama and Arizona.
Deaths
Georgia’s new death rate increased 10% in the most recent report, but we are still far below the national average death rate (which is very high).
References
https://covid.cdc.gov/covid-data-tracker/#vaccinations
https://wonder.cdc.gov/controller/datarequest/
https://drive.google.com/file/d/1errDPuX-_1bLUxqatYIyW2xEJmZYsHcA/view?usp=sharing
https://covid-gagio.hub.arcgis.com/
Georgia COVID-19 Updates is a free newsletter that depends on reader support. If you wish to subscribe please click the link below. There are free and paid options available.
My Ph.D. is in Medical Microbiology and Immunology. I've worked at places like Creighton University, the Centers for Disease Control & Prevention and Mercer University School of Medicine. All thoughts are my professional opinion and should not be considered medical advice.






Amber, on pushing legislators for additional funding for our public health resources here locally. I am assuming we need to reach out to our federal representatives? Or should I write to both the state, local and federal representatives?
As an aside, your work is so deeply appreciated. My internal medicine doc husband checks your updates like clockwork. Thank you for doing this data collection and analysis during this pandemic and sharing it with us all!