The Daily Digest, 03Feb2021
Georgia COVID-19 Updates
Vaccine Update
I think a lot of people are assuming that the reported vaccine efficacy for the Johnson and Johnson vaccine (66%) at 28 days post-immunization means its not as good of a vaccine as the Pfizer and Moderna ones. I think this is more of an artifact of the timing of data collection. So I think it’s helpful to lay out the timelines and findings in the graphic below. The two EUA-vaccines are depicted above the timeline and the yet to be authorized Johnson & Johnson vaccine is below the timeline. There are two arrows for Pfizer and Moderna to represent the two vaccine doses.
The percentages cited here come directly from the FDA Emergency Use Authorization briefings by Pfizer and Moderna or the Johnson and Johnson press release. We don’t make policy decisions based on press releases, of course, but this is what we know for now. Hopefully we gain greater clarity when the Johnson and Johnson vaccine goes up for EUA with the FDA. When you line the vaccines up this way, we see that the Moderna from the Johnson and Johnson vaccines are comparable as of day 28 (and actually, Johnson and Johnson is better at that time). The second doses of the Pfizer and Moderna vaccines eventually lead to a ~95% reduction in cases and 100% efficacy against severe infections (i.e. warranting a hospital admission). But after day 28, the Johnson and Johnson vaccine shows similar efficacy in preventing hospitalizations as the other two vaccines. And those dates on the timeline more or less align together. Another way to summarize this information is this table I saw on Twitter.
In the end, the two authorized vaccines and the others in development are so far showing incredible efficacy for preventing the most severe cases of COVID-19. There have been no hospitalizations and no deaths from COVID-19 after completing the vaccination series in these clinical trials. Compare that to what we know COVID-19 does in a similarly sized population. In addition, there have been no deaths that have been linked to any of these vaccines following investigation. Death is not the only vaccine safety metric, of course, and hopefully we learn more about serious adverse reactions as they are investigated in relation to the vaccine. But so far, this is a whole lot safer way to achieve herd immunity than allowing COVID-19 to burn through our population unchecked.
So when it comes to which vaccine you should get, I would say get the first one that is made available to you, especially with the variants that threaten us with a new surge. I’m just not sure this is the time to “shop around.” By the time you would need to wait to be considered “immune” from the two-dose vaccines, the efficacy data is essentially equal for the single dose Johnson and Johnson vaccine. Where I think the Johnson and Johnson vaccine will make its most dramatic impact will be in vaccinating rural or medically underserved communities where storage conditions favor a refrigerated vaccine (rather than a frozen one) and where it might be harder to follow up with the second vaccine dose required for the RNA vaccines.
For those who might have concerns that the vaccines were developed too fast, the Johnson and Johnson vaccine has a lot more research history than the RNA vaccines. A similar vaccine using the same technology was recently approved for them to protect against Ebola, going through the full European Commission approval process. And the clinical trials for the Ebola/adenovirus vector vaccine included examining safety in children. So if you’re afraid of something that is “too new,” then perhaps you will have greater confidence in the Johnson and Johnson vaccine technology that went through the traditional approval pipeline. The only difference is they replaced the Ebola component with the SARS-CoV-2 component.
I realize that I’m spending a lot of time here talking about the Johnson and Johnson vaccine and I should note that I receive no funding from Johnson and Johnson and am not endorsing any one vaccine. This is just meant to provide information to reassure and empower you as you make decisions regarding your vaccination plan.
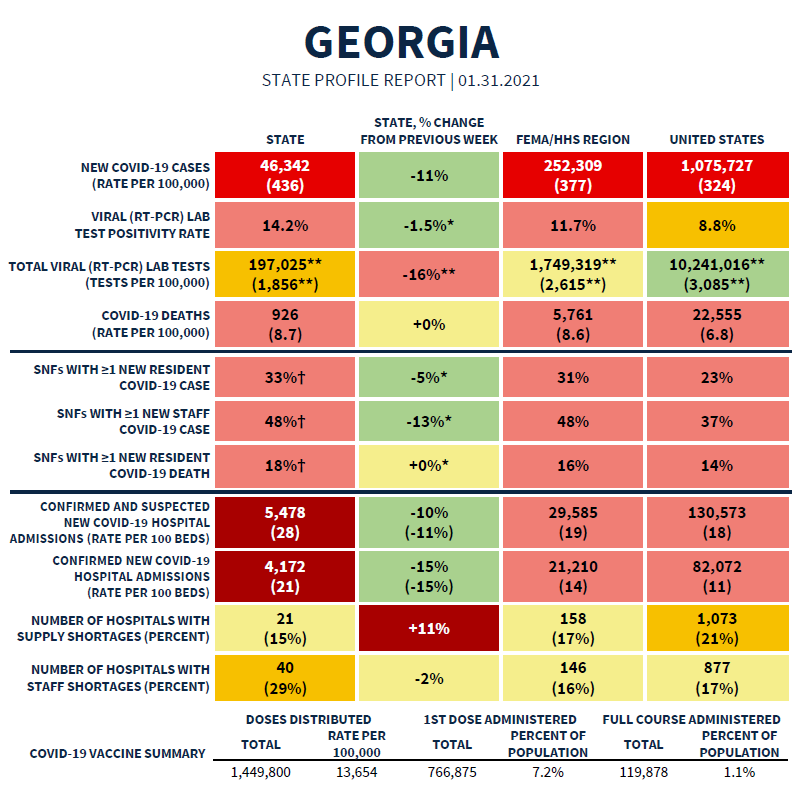
Moving on, we’ll next discuss the most recent State Report from the White House. The summary table is provided below. The full report can be found here. Georgia is still in the red zone for most metrics, but we do see signs of improvement. On the other hand, we did see an 11% increase in hospitals reporting supply shortages in the past week. The state is still in the yellow zone, but it’s something to keep an eye on.
According to this report, Georgia has the following rankings:
#5 for new cases per 100,000 (red zone, this report does include antigen cases in their calculation)
#5 for test positivity (light red zone)
#4 for hospital admissions per 100 beds (dark red zone)
#11 for new deaths per 100,000 (red zone)
Testing
Now that January is over, we can continue our look at how each part of Georgia is doing at testing its population. And today I want to spend a little extra time talking about how important testing is in the overall effort to control this pandemic. First, let’s look at the percent of PCR tests that were positive for each county type.
We can see that the percent positive rate rose dramatically between November and December and then the increase remained but slowed down into January. And whereas nonrural, rural and Atlanta suburb counties were very close together, they were about 43% higher than the rate seen in the Atlanta counties of Fulton and DeKalb. Ever since June 2020, the positivity rate for Atlanta counties has been below the rest of the state and not by a small margin. Atlanta more or less met the same positivity rate it saw during the summer surge (see July). However the positivity rate in January surpassed the peak set in July for the remaining county types. Here’s why the percent positivity rate matters: it’s an indication of whether we are testing widely enough that we are unlikely to be missing many of the COVID-19 cases that contribute to ongoing community transmission. The goal is to be at or below 5% for a sustained period of time. The higher you are above that 5% goal line, the more cases you are likely missing. Atlanta counties were below that 5% goal line for September and October.
So the answer to driving test positivity down is to do more testing and that’s exactly how Atlanta has succeeded in having the lowest positivity rate in the state and the lowest case rate per 100,000 in the month of January too. That’s because the more widely you test, the easier it is to see the positive cases and isolate them, preventing further spread. In the graph below you can see the test rate per 100,000 in the blue bars. The state average is on the far right. Atlanta is doing testing at a rate that is 34% higher than the state average and 62% higher than rural counties.
By comparison, the January case rate per 100,000 was lowest in Atlanta at a rate that was 19% below the state average and 26% the highest case rate counties (Atlanta Suburbs).
And when you have a smaller case rate, that tends to correspond to a lower death rate too. The cumulative death rate for different county types in Georgia is shown below, with data current as of today. The Georgia average is on the far right. The cumulative death rate is lowest in Atlanta counties and their death rate is 30% lower than the state average and 52% less than the leader (rural counties).
Testing and contact tracing is just one part of keeping this pandemic in check along with vaccinations, government interventions and community efforts to limit disease transmission. And while Atlanta still has a higher case rate than we’d like in the winter surge, it is an example for other parts of the state to follow. In summary, Atlanta’s aggressive testing output has likely saved a lot of lives.
This most recent week, the White House state report noted that Georgia decreased testing output by 16% and it is 40% below the national average. Based on the 01Feb2021 HHS Community Profile Report, Georgia is now ranked #46 in the nation for tests performed per 100,000 residents and only 76% of tests are being reported within 3 days. Unfortunately, the state is moving in the wrong direction right now in terms of testing. Part of this is due to the shift of personnel from specimen collection at testing centers to vaccination sites. There simply aren’t enough people to do all the things we need to do right now. But with the more transmissible variants in the US and in Georgia, I think it’s very possible that we’re going to see cases and test positivity climb again in the next several weeks. And when that happens, Georgia may be more blind to it than other states because of our deficiencies in testing.
Today, Georgia reported 30,175 new PCR test results, 11.8% of which were positive. Unfortunately, we don’t get to see demographic data from the state for antigen-identified cases nor how those positive cases compare to all antigen tests performed. But as the graph below clearly shows, the antigen test is an important part of the effort to identify cases.
Cases
The Georgia case rate per 100,000 is now 34.5% higher than the national average but the case rate for both is decreasing. The map below comes from the White House state report for Georgia. You can see that things are still very intense for the South. In fact, our neighbor, South Carolina, is ranked #2 for new case rate and Alabama to the west is ranked #9. It’s a precarious place for Georgia to be right now, with the arrival of the more transmissible variants of the virus. We really need to be doing more as a state and as communities to limit disease transmission and bring our case rate down as fast as we can. This could include mask mandates, limits or suspension of indoor dining, indoor occupancy restrictions, etc. Because our hospitals are already strained, even as we are continuing to decline right now. If we reverse this momentum before we return to pre-winter surge baseline, I really think our hospitals will be in an even worse situation. Yes, we are vaccinating some of the people most likely to require a hospital bed. But the more transmissible variant will mean more “shots on goal” for all age groups, including those we are not currently vaccinating. You can read more about the “shots on goal” idea here.
Today there was a net increase of 4924 newly reported cases (3816 by PCR and 1108 by antigen test). Forty percent of the newly reported cases came from nonrural counties outside of the Atlanta metro, 29% came from Atlanta suburb counties, 23% came from rural counties and 13% came from the Atlanta counties. As our case rate has decreased, we’re starting to see signs that contact trace investigators might be better able to manage the workload because we’re seeing negative numbers in the “unknown” category for cases by county.
The 7-day case rate per 100,000 continues to drop and now stands at a rate that is 29% above the summer surge and 52% less than the winter surge peak. But we still have a long way to go to get back down to the pre-winter surge level.
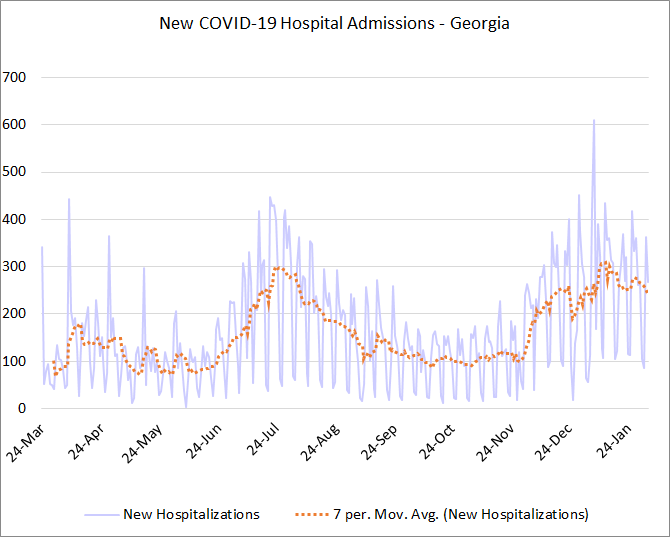
Hospitalizations
One thing that has stood out to me in the White House state reports has been the percentage of Georgia hospitals that are reporting staff shortages compared to the national rate. Things are declining for this metric for the US, but has held steady (and high) for Georgia.
Today Georgia reported 268 new hospital admissions for COVID-19 and 32 admissions to the ICU. The Georgia Geospatial Information Office COVID-19 Data Hub dashboards for patient census and hospital bed and ventilator capacity have not updated since 2/1/2021 at 11:00 pm. So I don’t have new data to report on how many patients are currently hospitalized nor how many ICU beds are occupied. I’ve notified my colleagues on the state’s data task force that there’s a problem, but since the team has been stood down, everyone has to work on their main job responsibility and there is no one really dedicated to curating the data full time. As I’ve said in previous posts, we need for public health (and especially authentic public health data) to be a bigger priority for state leadership.
But whereas the cases have dropped rather dramatically since the winter surge peak, the COVID-19 hospital admissions have not dropped as quickly. In fact, they remain in a bit of a plateau. This is also a departure from the way that the summer surge and descent took place.
Deaths
The graph below shows how Georgia’s death rate has trended over time compared to the US death rate from COVID-19. The national death rate has stabilized (thank goodness) and so has Georgia’s. But the Georgia death rate has stalled at a level that is 28% higher than the national rate. Hopefully we’ll see this death rate decline in coming weeks.
I made mention in the top of this newsletter that Georgia is ranked #11 for new death rate per 100,000. But things are even worse for our neighbors with Alabama ranked #1 in the US, South Carolina ranked #4 and Tennessee ranked #5.
Today Georgia had a high death total that has unfortunately become our new “normal” over the past couple weeks. There were 135 newly reported confirmed deaths today and 2 probable deaths. The probable deaths are those that don’t have a PCR test to confirm COVID-19, but had an antigen test or no laboratory data at all, but their manner of death was consistent with COVID-19. Some of these are recent, some of them are the result of investigators at DPH combing through death certificates.
I think that’s it for today. Enjoy your evening!
References
https://beta.healthdata.gov/Community/COVID-19-State-Profile-Report-Georgia/xhcs-tqqe
https://www.jnj.com/johnson-johnson-announces-single-shot-janssen-covid-19-vaccine-candidate-met-primary-endpoints-in-interim-analysis-of-its-phase-3-ensemble-trial
Pfizer EUA briefing document: https://www.fda.gov/media/144245/download
Moderna EUA briefing document: https://www.fda.gov/media/144434/download
https://www.jnj.com/johnson-johnson-announces-european-commission-approval-for-janssens-preventive-ebola-vaccine
https://beta.healthdata.gov/National/COVID-19-Community-Profile-Report/gqxm-d9w9
https://amberschmidtkephd.substack.com/p/the-daily-digest-01feb2021
https://dph.georgia.gov/covid-19-daily-status-report
Georgia COVID-19 Updates is a free newsletter that depends on reader support. If you wish to subscribe please click the link below. There are free and paid options available.
My Ph.D. is in Medical Microbiology and Immunology. I've worked at places like Creighton University, the Centers for Disease Control & Prevention and Mercer University School of Medicine. All thoughts are my professional opinion and should not be considered medical advice.