Things continue to deteriorate
This week all metrics continue to rise for COVID-19 in Georgia and across much of the South. But because Georgia is home, it’s getting the focus today. Unless otherwise stated, all data presented originate from the Georgia Department of Public Health. If you’re new to the newsletter, I just generate the data visualizations and show you how to read them and what I see in the data.
Cases rose 29%; we haven’t seen >40,000 cases in a week since the last week of January 2021. There are no signs this is slowing down.
Deaths rose 34%
Hospitalizations rose 17%
ICU admissions rose 47%
Test volume and test positivity continues to rise for both the PCR test and the antigen test. However, the rise in test positivity shows some sign of slowing down. That makes sense. High test positivity is a sign that we’re not doing enough tests. If we increase testing volume, we should expect test positivity to flatten or improve.
The US Department of Health and Human Services generates a Community Profile Report that helps us to see a lot of data that might not be available from the Georgia Department of Public Health. The graph below is built with data from that report, helping us to see how test positivity varies by age group. The goal is to be at or below 5%. All age groups are well above that goal line. So Georgia is missing a lot of tests.
And test positivity is highest among K-12 aged children. For 12-17 year olds 1 in 4 PCR tests is positive and for 5-11 year olds it’s just above 1 in 5 tests that are positive. Georgia isn’t testing any age group enough, but it is especially missing cases in children. Those children are vectors of disease, able to transmit to others. And they live in families, sometimes multigenerational ones. So we should all be very alarmed by the increase we are seeing both in cases among these pediatric age groups (more to come below) as well as the state’s decreased ability to identify cases (high test positivity).
But let’s start with the bigger population when it comes to case rate per 100,000. The state’s case rate has risen 1390% since July 1. It is rising fastest outside of the Atlanta metro.
Cases feed both hospitalizations and deaths. I’ve been discussing the strain on hospitals a lot on Twitter and encourage you to see the impacts there. I have limited space in today’s newsletter but I tweet nearly every day about the strain on hospitals.


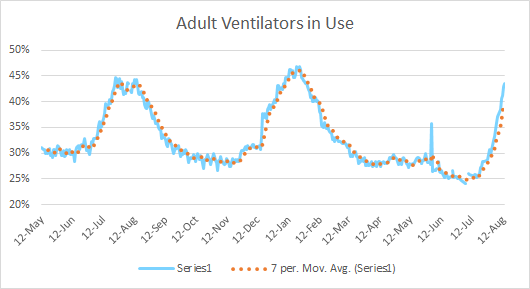
Today, for the first time since last winter, Georgia’s patient census tops 4000. And while the state hasn’t yet reached the patient census record set in January 2021, it is close to reaching the record for adult ventilator use.
There are a lot of people in the hospital for COVID-19. But while the state hasn’t yet reached the previous peak set in winter 2021, it is approaching that maximum for adult ventilator use. So people seem to be sicker this time around, needing more advanced care.
The other thing that is alarming is the steady increase we’re seeing for hospital admissions among 18 - 49 year olds. So as much as younger adults may have been lulled into a sense of complacency, believing that COVID-19 isn’t that bad for younger adults, it’s clear from the data that 18 - 49 year olds are not invincible. Not to mention that these hospitalizations come with significant financial costs that add to already existing economic strain for people trying to pay student loans, etc. Meanwhile, the vaccine, a lifesaving tool, is free.
There is a delay, however, in case surges compared to deaths. The graph below is one I don’t show very often. It shows the cumulative count for cases (PCR + Antigen) and confirmed deaths, on separate y-axes. We see this trend where cases surge and then deaths climb too, just later on. Cases have been building for weeks. But last week was when deaths started to rise too. This week, you can start to see that increase make a visible difference on Georgia’s already large death toll.
A special focus on kids in Georgia
The news these days is full of stories about children’s hospitals filling up in other states and schools in Georgia transitioning to virtual learning due to outbreaks. So let’s take a look at what’s happening with pediatric populations.
The graph below shows the weekly PCR case totals by age group for Georgia over the past 8 weeks. See if anything stands out to you.
All of the age groups are seeing increases. Most age groups are seeing similar or smaller increases this week than they saw in previous weeks (see 30-39). But where we are seeing an expansion in the number of cases detected is in 10-17 year olds, even as this age group has the highest test positivity in the state. So as intense as this week’s case increase appears, it is likely a vast undercount of what the real disease burden is for this age group.
The Georgia Department of Public Health also produces a weekly report for School-Aged Surveillance Data. The data presented in this week’s report are striking. Below, the graph on the left shows the weekly case count among K-12 aged children. The state has already matched the previous record, with the largest increase seen in 5-10 year olds (elementary aged children). It’s the biggest weekly total for this age group recorded since this report began. Meanwhile, I also want you to notice that the rise for this surge is far faster than what we observed in the winter surge. We are seeing the combined effects of a much more transmissible variant and the return to school with poorly thought out disease mitigation strategies.
Not only are we seeing a rise in infected children, we are seeing that they are sick enough to need an ER visit in record numbers. The graph above on the right shows that every age group from 0 - 22 years of age, is seeing a percentage of ER visits due to COVID-19 illness that meets or exceeds previous records set last winter.
The bar graph above shows infections among school-aged children, but does not necessarily link those cases to the school environment. However, the graph below (also produced by Georgia DPH) tells us that the most recent week of reporting shows a record number of outbreaks for both daycares and schools. Bear in mind that DPH does not distinguish between public and private K-12 schools and this graph also includes college/university outbreaks.
I went “mama bear” in a previous newsletter on this topic, predicting exactly what we are seeing now. It stinks to be proven correct. But I hope that school superintendents and parents can wake up to the reality that the virus does not care if they don’t think this virus is a big deal or if they are ready to move on because “people die every day.” The reality is that you can’t keep in person learning if you have widespread absenteeism among students, faculty and staff. It is far less of a hassle for schools, teacher, children and their families to take steps to reduce disease transmission in the schools (i.e. mask requirement, social distancing, improved ventilation, etc) than to go through multiple transitions to virtual learning. Hopefully, when these schools come back to in person learning, the superintendents will have made a different choice to adopt a culture that prioritizes student safety so that they can learn in the best setting possible.
But beyond the logistical problems, it is morally bankrupt to claim that wearing a mask is a personal choice when the risk of that choice is not limited to the individual making that choice, but harms so many others. It is a choice that tells others that even as cases surge and hospitals are at capacity, the person does not care if others get sick, go to the hospital or die, and cares even less if they themselves are the cause of that suffering. Who raised these people to care so little for others? Why would you want your children to behave that way? It really is similar to the harms posed by second hand smoke. A person can make that choice for themselves, but it poses significant harm to others. And that’s why we don’t allow smoking indoors with the exception of bars, not on airplanes and certainly not in schools. If someone lit up a cigarette in a school we would be outraged and maybe have some choice words to describe them. But we haven’t taken the position of “people die of lung cancer everyday” like the way COVID-19 is being described. Why would we take that same position on COVID-19? We have the tools and strategies to prevent mass suffering and death, to keep schools operational and parents able to work and feed their families. Not using those strategies is heartless, cruel and logistically not sound. It stalls our return to normal, rather than accelerating it as some people seem to think. You cannot “rip off the bandaid” with the delta variant. It will find every unvaccinated human it can find (and even a few vaccinated ones). Unfortunately, when we gather unvaccinated children in a school and don’t take basic measures to protect them, we have invited the virus to a buffet. This was an unforced error.
We are going to see the grandparents this weekend because one of them is having a milestone birthday. My family of four took a home antigen test today before we left, to ensure COVID-19 wasn’t coming with us. Three of the four of us are fully vaccinated, but with delta and breakthrough infections, we aren’t taking unnecessary chances with Oma and Opa’s lives. Their lives are worth more than one weekend. I wish other people shared this basic humanity. I’m happy to report that we were all COVID-19 negative. You can pick up these home kits that are similar to a home pregnancy test - but no urine - at your local pharmacy or grocery pharmacy. We had results in 15 minutes.
But as we get ready to arrive at our destination, I’m going to sign off for now. Have a great weekend, make good choices and thank you for caring about the people around you.
The COVID Digest is a free newsletter that depends on reader support. If you wish to subscribe please click the link below. There are free and paid options available.
My Ph.D. is in Medical Microbiology and Immunology and I am Chair of the Division of Natural Sciences and Mathematics at the University of Saint Mary. I've worked at places like Creighton University, the Centers for Disease Control & Prevention and Mercer University School of Medicine. All thoughts are my professional opinion, do not represent the views or opinions of my employer and should not be considered medical advice.













Hi, Dr. Schmidtke. Your digest has been such a lifesaver for me during these tumultuous times. My husband is a doctor and is seeing the first-hand effects of this virus and continued vaccine hesitancy and mask angst. Your words, expertise, and digest have helped me write letters to get one of our children's schools to require masks. Our headmaster has even quoted you now in some of his messages! I consistently tell people masks and vaccines are medical, not political. I work hard to listen to people's concerns and then to calmly answer them with facts and science. It's been draining, but it's also been rewarding. Just today I had a former babysitter of ours who is pregnant with her third child tell me I've helped to convince her to get vaccinated. I can't imagine how exhausting your work is - but hopefully, it's rewarding as well.
At any rate, here's what I'm struggling with right now. I know how busy you are, but I have some friends and people on social media who follow me who are genuinely trying to sift through the heaps of information (and misinformation!) out there and make a prudent choice for their families. I am trying to address their vaccine hesitancy in charity and with facts. One argument I've heard several times is how vaccinations were initially billed as a public health measure (which they still are in my view, of course), but that now people are seeing that the vaccines only reduce one's own symptoms and that people with the vaccines are still spreading the virus, so why bother taking the risk of getting vaccinated? These same people, unfortunately, think the risk of vaccines is a real threat and have misguided fears and seek out YouTubers and Instagram influencers who incorrectly use VAERS data to scare people. Well, I've tried to explain when they question the efficacy of the covid vaccines that while there are breakthrough infections, they still remain quite rare. These same people don't understand why I'm wearing a mask even though vaccinated (or sadly why people mask-up at all). I explain that I'm currently wearing a mask as an extra mitigation measure since delta is proving to be highly transmissible. One individual told me her research has shown that there's only a negligible reduction in transmission among vaccinated individuals and she asked me for research saying otherwise. She feels getting the covid vaccine remains a mostly a personal protective decision and only potentially protects others while the individual assumes all the risk of the procedure. I've tried to explain how increasing vaccine rates reduces transmission and the chance the virus will continue to mutate. I've also offered CDC statistics on how effective the vaccine has been and how rare side effects are to assuage her concerns about the "risk of the procedure." She also doesn't seem to grasp that reducing symptoms - even if the vaccine doesn't always block infection - is still a major feat and is dramatically reducing death. She wrote, "Without a sterilizing vaccine, the virus will never be eradicated, which makes it seem less of a community-driven decision and more personal as well. Personally, my primary care doc, an MD, said he cannot recommend it for me. So I'm genuinely trying to figure out honest to goodness research because I know science is changing and new research continues to be performed, and I want to be sure I am being a charitable Christian while also making wise stewardship decisions for my own family's bodies. Does he have any insight or research articles I can analyze?" I'm not a virologist (obviously!) or a doctor (though my husband is!). I was, however, a medical journalist for nearly a decade (before switching writing gears after becoming a mom) and I truly want to help bust vaccine myths and rewrite the false narratives circulating around. I know some people are going to be very hard to ever sway, but people like this woman are willing to listen. So is there any chance you could provide me with some links, research, etc. that would help answer her (somewhat convoluted) question? I understand if you don't have the time to address this, but maybe even another expert reader might be able to offer me some resources. Thanks for the tireless work you're doing. You truly are a lifesaving hero!
Thanks for calling out ventilation. That gets so little focus and, I feel, could be a significant improvement in our response (just compare the relative safety of outdoors and, dare I say, airplanes). Even a single open window can help, especially since the dose makes the poison for this disease. And, if we get serious about ventilation in the long run we may even reduce the burden of other (current or future) respiratory viruses. It also empowers individuals, who can test how risky a particular room is with a personal co2 detector.