This week we saw an abrupt change in the guidance regarding masking from CDC. Along with countless other public health professionals, I strongly opposed the first change that came in May. You can read my reactions to the May guidance change here and here. I’m not here to write a newsletter filled with “I told you so” or dunk on the CDC. What’s done is done. But I want to go through the data that drove the decision to change the guidance this week because the data help us to see how big the problem is.
You can review the leaked slides that influenced this decision here. Please note that many of the slides have disclaimers that say they represent preliminary data that are subject to change. I should also note that we don’t have the benefit of the audio of this presentation. Whereas CDC’s public communications about the pandemic have been disappointing at times, their cadre of scientists and epidemiologists includes some very talented communicators. We are not able to suss out their intent, the context and nuance they provided, etc.
First, we need to define a breakthrough infection. These are infections that take place among people who are fully vaccinated (as in 2+ weeks since their second dose of mRNA vaccine or since receiving the Johnson and Johnson vaccine). Infection is also different than illness. Infection is testing positive. Illness is experiencing symptoms. This will be important later in the newsletter when we talk about viral load among those infected after vaccination.
The CDC did a weird thing in May where they stopped tracking breakthrough infections for the public and only tracked hospitalizations and deaths among the fully vaccinated. But this week Georgia Department of Public Health began providing information regarding breakthrough infections, including those that didn’t require hospitalization or result in death. The data run through 27Jul2021. Of the 4.14 million Georgians who are fully vaccinated, 0.12% of them have tested positive, 0.003% have needed hospitalization for COVID-19 and 0.0006% have died from their COVID-19 infection.
We should anticipate that this is likely an undercount of breakthrough infections, given that CDC doesn’t recommend testing fully vaccinated people after exposure unless they’re experiencing symptoms. But based on what we do know, we can see that infection after vaccination is very, very rare. Among those who do test positive, their hospitalization rate is 2.4%, about half of the state’s average hospitalization rate (5.7%), and their death rate is 0.49% compared to 2% for the state average. In other words, the cases that do happen after vaccination are not nearly as severe (on average) compared to the unvaccinated population. Another big thing to point out here is that we only have these data because of contact tracers. So big thanks to the people doing this important work. And please be sure to answer these phone calls if/when you are called. We all benefit from more robust data.
The Georgia data align well with what CDC was seeing elsewhere. Using data from the UK, they estimated that the vaccine resulted in an 8-fold reduction in infection, but a 25-fold reduction for both hospitalization and death. So as an average vaccinated person, you are 25 times less likely to die from COVID-19 than an unvaccinated person, and 25 times less likely to end up in a hospital. Hopefully that provides a lot of reassurance.
But many of us don’t live in isolation. We may live with people who are unable to be vaccinated (i.e. kids under 12), immunocompromised or who have underlying medical conditions. And one of the big motivations we had for getting vaccinated ASAP was interrupting possible transmission to those affected loved ones. Being 8 times less likely than an unvaccinated person to test positive is still pretty good for a vaccinated person, but it’s important for us to be aware that delta has exposed a limitation for the currently available vaccines and take steps to overcome that.
Using a study of healthcare workers in the US, the CDC was able to see breakthrough infections through 10Apr2021 (before delta got going in the US). But for those who were at least partially vaccinated, their viral load was lower, they had a shorter period of time where viral RNA was high, were much less likely to have symptoms like fever and had a shorter duration of illness. A paper like this likely contributed to the May guidance change. But again, it was before delta arrived.
There’s also growing evidence that vaccine effectiveness is reduced among immunocompromised populations. In one study, vaccine effectiveness of mRNA vaccines against hospitalization was only 59% for the immunocompromised, compared to 91% among those who were not immunocompromised. This study collected data through 10May2021, when delta was in the US but not gaining steam yet. In the same time frame, there was reduced vaccine effectiveness (70-75%) among nursing home residents, according to the CDC slides.
Taking all of these data points together, this slide nicely summarizes how communications can and should change when it comes to the vaccine.
Then the slides transition into talking about delta. So all of that reduced effectiveness stuff discussed up to now was based on the pre-delta stage of the US pandemic experience.
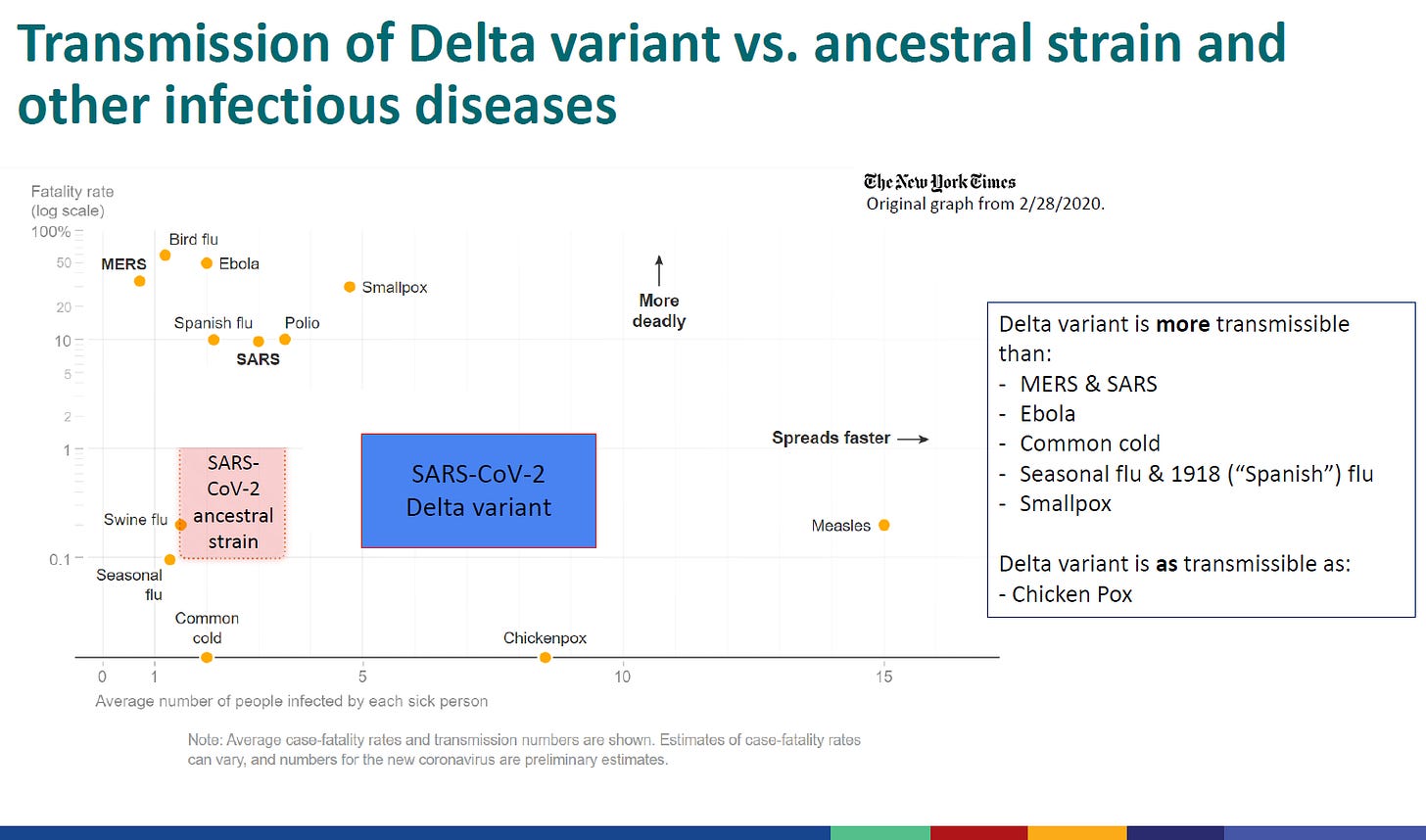
To me, the slide below was the most impactful slide of the whole slide deck. It compares the transmissibility of the original SARS-CoV-2 virus (causes COVID-19) and the delta variant of SARS-CoV-2 to other illnesses. The y-axis shows the fatality rate. The x-axis shows the average number of people infected by each sick person (this is sometimes described as R0). Thankfully, COVID-19 in both forms is not as deadly as many of these other viruses. And also thankfully, some of the deadliest diseases aren’t very transmissible. But this modified graph helps us to make some useful comparisons. The delta variant is more transmissible than both seasonal and 1918 influenza (<-the so-called “Spanish flu”), Ebola, Smallpox and other serious coronavirus diseases MERS and SARS. I am assuming that the blue box for delta is meant to represent a range (this is a place where having the audio of the presentation would be helpful) and if that’s the case, the delta variant is estimated to have an R0 in the range of 5 ~9.5? This puts the delta variant on the same scale as Chickenpox.
That will mean something to people of a certain generation. But the US has had a pediatric vaccine for chickenpox since 1995, resulting in a 93% decrease in infections since the mid 1990s. It will mean something to parents but maybe less to young adults and teens because they’ve never lived in a world where chickenpox quarantined entire grade levels of their elementary school and schools shut down to decontaminate. Honestly, hearing that a deadly disease is as contagious as chickenpox puts a lump in my throat.
I’ve previous discussed the numbers related to a higher R0, but sometimes we benefit from visuals. I made the graphic below to show us what happens with just three chains of transmission comparing the original (ancestral, orange) version of the virus compared to the middle of that range that CDC is estimating for the delta variant (blue).
With the ancestral version of the virus, on average a sick person would go on to infect two more people. Each of those people would go on to infect two additional people, etc, etc. By the end of three transmission events, you’d go from one sick person to 8 people. For delta, if the R0 is 7, then things escalate much more quickly. One person goes on to infect 7 people. Each of those 7 go on to infect 7 more (for 49). Each of those 49 people go on to infect 7 more people, resulting in 343 infections by the end of three transmission events. It’s a 419% increase in infections over the same period of time for delta compared to the ancestral virus.
This next slide from CDC includes some evidence that suggests why delta is so much better at spreading. First, we need to talk about how PCR testing works. PCR is essentially a big photocopier of nucleic acid. It uses primers that we can think of like RNA or DNA sequence magnets specific to SARS-CoV-2 virus and if those lock on to the sequence they’re looking for, the photocopier starts making lots of copies after an intermediate process where the RNA between the primers is reverse-transcribed into DNA first. To summarize, the primers find their target sequence (viral RNA), the RNA between the primers is copied into DNA and then loads of copies of that DNA are made. In the diagnostic test for SARS-CoV-2, the DNA copies are also fluorescent. When there is enough fluorescence generated because there are sufficient copies of target DNA, then it crosses the signal threshold at which the fluorescence can be detected (also known as a cycle threshold or Ct). If you have a lot of the original target sequence in a sample, the photocopier will reach that fluorescent signal threshold faster (a low Ct) than if there were only a few copies of the original target sequence. There are two caveats I should point out: (1) the primers do not discriminate between viral RNA that is part of a viable viral particle versus the mess of RNA that’s left over after one of your T cells kills a virus-infected cell (unable to start another infection). (2) You can have laboratory errors that impact the Ct, such as adding too much or too little sample.
The first bullet on this slide talks about how breakthrough cases from delta compare to non-delta breakthrough infections. On average, the delta breakthroughs had a lower Ct value, suggesting that the original amount of target RNA in the fully vaccinated person infected with delta is bigger than those infected with non-delta variants. This might suggest that those infected with delta after vaccination have a bigger viral load. Though, we should remember that they could be measuring “dead” viral RNA too.
The second bullet talks about how long the laboratory test can reliably detect viral RNA in a delta-infected person. This means they are possibly contagious for longer than with previous variants of the virus.
The third bullet talks about delta infections not after vaccination but after previous natural infection. It compares the alpha (formerly known as the “UK variant”) to the delta variant. If a person was infected more than 6 months ago, they are about 1.5 times more likely to get reinfected with delta than with alpha.
Taking all of this together, we can see that both those previously infected and those previously vaccinated can get infected with delta. The delta variant appears to be more transmissible because it produces a much larger viral load (this increases how much virus a person exhales) and for a longer period of time than previous variants.
This next slide has gotten a lot of buzz too. The first bullet point really sort of goes with the previous slide. But the second bullet point is the buzzworthy one. It describes an outbreak in Massachusetts that did have breakthrough cases. What they found was that the average Ct value among the breakthrough infected people was the same as the average Ct value for those who weren’t vaccinated. That might mean that they have approximately the same viral load.
If we take this together with everything else presented so far (including the Georgia data), here are our major takeaways:
Infection after full vaccination is still really rare, considering how many people are fully vaccinated. Even among those who do have a breakthrough infection, they still have substantial protection against hospitalization and death compared to someone who is unvaccinated.
Of those rare folks who do have a breakthrough infection after vaccination, they appear to carry the same viral load as a person who is not vaccinated. Therefore, it is reasonable to hypothesize that they can transmit to others. Again, we don’t know how much the PCR is picking up on “dead” viral RNA, but let’s be more cautious than not.
Delta is more transmissible because of the sheer volume of viral particles produced and a longer duration of that high viral load compared to previous variants.
Next, let’s understand why this leads to discussions regarding masking and who should mask and use other non-pharmaceutical interventions (NPIs). They did some modeling here, which is sort of like a simulation that estimates outcomes based on certain assumptions or criteria. They took the low end estimate of vaccine effectiveness (remember those long term care facility and immunocompromised studies from above), assuming that only 50% of infections are being detected and reported. Then they estimated what happens when no masks are worn, when only the unvaccinated are masked and when everyone is wearing a mask. The blue dashed line represents what happens if 60% of the population is fully vaccinated (US s currently at 57.7% of total population with 1+ dose). It gives us an approximate for where we currently stand. The left graphs assume that only 5% have natural (non-vaccine) immunity whereas the right graphs assume that number is higher.
Let’s start by looking at the top graphs, which represent something similar to the alpha variant with an R0 of 2.5. On the left, if no one is masking (brown), the probability of a case rate increase at current vaccination rates is quite high, but reduced a by a lot if the unvaccinated are wearing masks (gold color). On the right, with a higher level of natural immunity in the community, then the probability of increase is quite a bit lower. Then let’s look at the graphs on the bottom. Look where the blue lines are. Having a policy of no masking ensures 100% probability of a case rate increase with a variant like delta (here’s looking at you, school districts). If only the unvaccinated are wearing masks, it reduces the probability but not by much if you’re in the graph on the left. We want to be at or below the horizontal dashed line, which represents a coin flip probability of risk. I might argue that our natural immunity is greater than 5%, and favor the graph on the right. This graph forecasts that if we mask everyone, we bring the probability of a case rate increase to between 0 and 25%. The other interesting thing about this slide is the numbers they give to estimate effectiveness of masking for the person infected (40-60%) and as personal protection (20-30% effective). Because we can’t tell who is infected and transmitted, we really can’t take the risk that they’re breathing out 1000 times more virus than before the delta variant took over. We need everyone wearing a mask for the time being and vaccinate as many people as we can as fast as we can in the meantime. Because look what happens to the right of the graphs…the more people are vaccinated, the more we can go to an only unvaccinated wear masks sort of strategy.
But to make matters worse, there’s evidence from other parts of the world that infections with delta (not considering vaccination status here) may be more severe than what we previously experienced with alpha or the ancestral strain. When you’re looking at an odds ratio (OR) something with an OR of 1 means the likelihood is the same. Above 1 and the odds are greater, below 1 and the odds are less. In Canada, they found that delta-infected patients were >2 times greater risk of hospitalization, almost 4 times greater risk of ICU admission and 2.4 times greater risk of death.
This is important. For a time, we were wondering if the reason it seemed like hospitalizations were going up was just because of a “shots on goal” sort of problem - more people are getting sick, so more people are going to the hospital. Instead, it’s possible that the increased viral load with delta is contributing to a more complicated disease course with greater frequency of severe outcomes. Considering how many children’s hospitals are filling up across the country, perhaps this is not a surprise but rather a humbling realization.
The presentation concludes with a summary slide that is not good news, but important for us to know nonetheless. We are not dealing with the same situation as we were a year ago. Yes, it’s still the SARS-CoV-2 virus, but it has evolved to become more contagious and likely more severe.
The vaccines remain really good at preventing hospitalization and death, but they may be less able to prevent infection or transmission as we had hoped. In the end, if we can keep infections minor and out of the hospital, that’s still a significant win. But we have yet to learn what this will mean for long COVID-19. It also means that the fully vaccinated are not invincible. We need to bring back non-pharmaceutical interventions (NPIs) like masking, social distancing, improved ventilation, etc. Vaccines are one of our slices of swiss cheese. They are one of our more powerful slices of cheese, arguably with fewer/smaller holes than the other strategies, but they need to be layered with other mitigation strategies until we can bring case rates down.
The faster we all row in the same direction and work together to limit transmission rather than pretending it doesn’t exist, the sooner we get to take a break from some of the strategies.
I will add that as the parent of a 10 year old who is too young to be vaccinated, I am losing sleep over what is going to happen to all of these kids across the country in delta-surging areas. Our school is going to require masks and he is really good at wearing a KN-95. But what happens at lunch time in a cafeteria full of kids who all take their masks off to eat, with a virus with an R0 of 7? If even one of those kids is positive (likely an underestimate), 7 kids will be positive 3-4 days later, 49 kids 6-7 days later, 343 kids 10-13 days later. The children’s hospital in my area is already full with COVID-19 and/or RSV patients and school hasn’t even begun. With a viral load 1000 times greater than for alpha the exposure time isn’t an accumulation over 15 minutes. It’s more likely to be counted in seconds.
FDA is promising to bring “all hands on deck” with staff working evenings and weekends to expedite the full approval of the COVID-19 vaccines. I am less concerned with getting full approval for the vaccines than getting EUA for kids under the age of 12. Although I don’t think it will convince that many people on the fence who haven’t trusted government up to now, full approval will pave the way for vaccine requirements and we DO need those for congregate or crowded settings (think schools). I know there’s a lot of burnout everywhere, but I wish very much that FDA was bringing all hands on deck to expedite the paperwork and bureaucracy of authorizing a vaccine for kids. I want my kid to have a fighting chance against a virus with an R0 of 7 that is likely more severe than its predecessors.
References
https://www.washingtonpost.com/context/cdc-breakthrough-infections/94390e3a-5e45-44a5-ac40-2744e4e25f2e/
https://dph.georgia.gov/document/document/covid-19-among-fully-vaccinated-people-graphic/download
https://www.medrxiv.org/content/10.1101/2021.07.08.21259776v1
https://www.cdc.gov/chickenpox/vaccine-infographic.html
https://www.washingtonpost.com/health/2021/07/30/fda-vaccine-full-approval/
The COVID Digest is a free newsletter that depends on reader support. If you wish to subscribe please click the link below. There are free and paid options available.
My Ph.D. is in Medical Microbiology and Immunology and I am Chair of the Division of Natural Sciences and Mathematics at the University of Saint Mary. I've worked at places like Creighton University, the Centers for Disease Control & Prevention and Mercer University School of Medicine. All thoughts are my professional opinion, do not represent the views or opinions of my employer and should not be considered medical advice.











Amber, do you think the higher RO value that is being seen with Delta is a result of a change in the virus or could it also be a change in our behaviors-the unmasking, going back into restaurants, going to "prepandemic" routines when we were just in a valley between surges? Do you think that range in the RO on the slide could come in on the low end with more responsible pandemic behaviors?
Finally, Blaine and I know this is a very busy time for you and we so appreciate you continuing to keep you share your knowledge with us. It helps so much!