Week in Review, 10-16May2021
Georgia COVID-19 Updates
Combined Data
The graph below shows how four of our big metrics for tracking the COVID-19 pandemic are tracking over time. Cases are represented by the blue line and correspond with the left y-axis. All other metrics correspond with the right y-axis. The reason I graph all of these things together is so that we can see the way these things trend together (or differently) over time.
All four metrics decreased this week, ranging from an 11% drop for hospital admissions to a 21% drop for new cases. There were only 103 newly reported deaths this week. During the summer and winter surges, we had higher daily death counts than that. So we’ve come a long way. Let’s hope this good run continues. We can help these trends to continue by getting vaccinated as soon as possible and doing what we can to limit disease transmission.
Testing
The PCR test output trend over time can be seen in the graph below, represented by the blue line that corresponds with the left y-axis. The red line represents the test positivity rate over time, and corresponds with the right y-axis. The gray dashed line is the goal line for test positivity.
We saw a 10.6% increase in PCR testing reported this week. Test positivity continued to decrease and the weekly test positivity rate was 3.7%.
Antigen testing decreased this week, by about 17%, but the positivity rate decreased to 4.4%.
The DPH does not provide data regarding demographic details for cases identified by the antigen test. Keep that in mind as we go through the demographic data in the following sections. You’re only seeing part of the data. Meanwhile, antigen testing identified 31% of the cases this week.
Cases
The number of combined new cases (by date of report) is as follows:
- 24 hours: 374 by PCR + 155 by antigen = 529 (+0.05%)
- 7 days: 3893 by PCR + 1750 by antigen = 5643 (+0.5%)
- 4 weeks: 21,402 by PCR + 9,927 by antigen = 31,329 (+2.9%)
This week cases were flat or decreased for all age groups except those 80+, who saw a 14% increase. That’s a bit worrisome considering they’re in the age group where the rate of hospitalization is 32% and the case fatality rate is 22.1%.
Hospitalizations
The number of new hospital admissions (by date of report) is as follows:
- 24 hours: 20 new COVID-19 admissions, 2 admission to the ICU (weekend reporting is typically light)
- 7 days: 468 new COVID-19 admissions, 93 ICU admissions
- 4 weeks: 2200 new COVID-19 admissions, 426 ICU admissions
As discussed in the combined data section, hospital admissions decreased this week, but not for everyone. Hospital admissions rose slightly for those 10-39 and 80+.
There are only two hospital regions in the yellow zone for COVID-19 patient census, regions A and F. Every other hospital region is in the green zone. For ICU bed usage, there are no hospital regions in the red zone. However, Region A (northwest Georgia) hit 100% ICU bed usage yesterday and added surplus ICU beds overnight to adjust. The surge on ICU beds there does not appear to be related to COVID-19 though.
Deaths
The number of new confirmed deaths (by date of report) is as follows. The percentage in parentheses indicates how the increase compares to Georgia’s cumulative total at the start of each window of time.
- 24 hours: 1 confirmed, 0 probable deaths
- 7 days: 103 (+0.6%), 36 probable deaths
- 4 weeks: 590 (+3.4%), 158 probable deaths
This week, deaths increased for those 40-59. Please work to get vaccinated - not only to protect yourself but the people you encounter.
Where do we go from here?
On Friday, I sent a message to one of my pandemic besties, another public health professional saying, “this is the hardest day of the pandemic since lockdown.” The previous day CDC Director, Dr. Rochelle Walensky, told Americans (and by virtue of CDC’s reach, the world) that vaccinated people no longer needed to wear masks and we could go to an honor system of masking in the public. It sent shockwaves through the public health field because of how poorly thought out both the words and roll out of the new policy was. It led to confusion and anxiety. It unintendedly gave cover to those who have been anti-mask, anti-vaccine, anti-pandemic this whole time to push their risk tolerance onto others. It put businesses into disarray, trying to figure out what to do to protect their employees while serving the public. But in addition, it signaled a new chapter in the pandemic with the predictable consequence that schools, businesses and jurisdictions immediately lifted their mask mandates. It may not have been intended, but the CDC Director effectively waved the white flag for the United States on the pandemic. People are moving on. I so wanted to celebrate this time with you when we could take the masks off, but it is too soon to celebrate. We have too few people vaccinated. I worry what the rush to return to pre-pandemic life will mean for the hard work we’ve done to bring cases, hospitalizations and deaths to the lows we see now.
I’ve been through the clearance process at CDC to publish public-facing material. Every word in public health communication matters. So before submitting an article for peer review to a scientific publication, the agency goes through its own internal peer review process with its science, data, and communications. It doesn’t matter how deep in the laboratory data or statistics you might be, every word you say is scrutinized for how the public will receive that information and possibly misinterpret it. Words are chosen to avoid that misinterpretation, to make it abundantly clear what the CDC is and is not saying. We have been able to see some of this play out in the public space this year by watching the Advisory Committee on Immunization Practices meetings. These meetings have always been open to the public, but only this year did the public tune in to live-tweet them. We have watched the members agonize over the decision to pause the Johnson and Johnson vaccine, forecasting the impact it would have on domestic as well as international vaccination rates. They debate for hours, pouring over antibody titers, case rates, racial disparities, risk ratios, and polling data to gauge public sentiment.
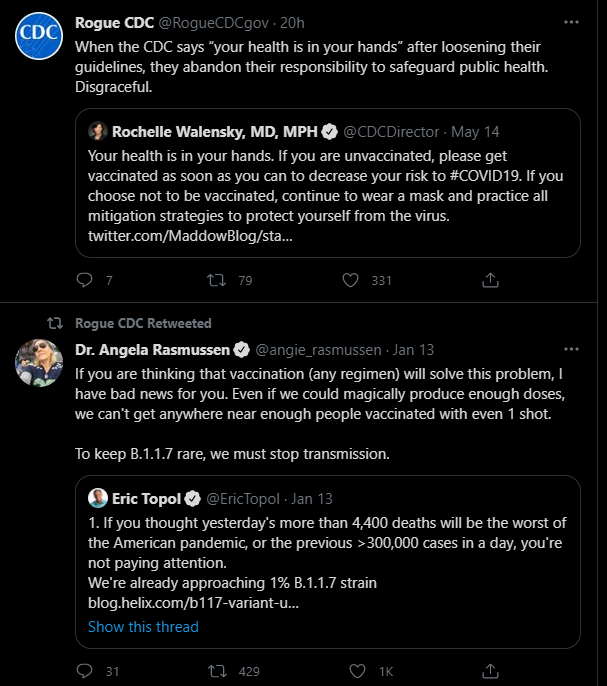
But this decision didn’t seem to get the same scrutiny. The decision caught not only public health professionals but even the White House off guard. When the CDC rolls out policy changes, its websites are coordinated to reflect the new guidance almost immediately. There are still pages that don’t reflect the new guidance, indicating that this was not a coordinated decision - the rank and file of CDC were not part of this. In the past administration, we saw a number of “rogue” accounts for various federal agencies pop up on social media, trying to speak up for a work force who was afraid to speak out but knew something was wrong. The one for CDC was silent after January 13th 2021, but began tweeting again after the Director’s decision this week. When you have good morale in your organization, this sort of communication is not needed.
Even as the CDC Director spent the morning today walking back and clarifying her comments on the Sunday morning talk shows remotely from Massachusetts (CDC headquarters is in Atlanta), her agency is operating at 25% staffing on the property at any given time, and only for essential duties. What would you guess the vaccination rate is for CDC employees and contractors? I would bet it’s pretty high. Probably even as high as the anticipated herd immunity threshold. So if the CDC Director doesn’t think her agency should return to full capacity with high vaccination rates, why is she recommending unmasking for the general population with lower vaccination rates? If it is not safe for her workforce, then why is it safe for you? How does this improve public trust in the Centers for Disease Control and Prevention? It hurts to even write this, given my fond memories of working there.
It’s unclear at this point whether this was an example of political interference, unilateral decision making, or just a faux pas in communications. There’s support for each of these scenarios. With respect to possible political influence, the Biden Administration had social media content ready to deploy following the announcement. Was that pre-coordinated? Or something they had worked on and set aside for the eventual time when mask guidance would be lifted? Was this a unilateral decision by the Director? The consequences we’ve already seen from the guidance change were predictable and would have been identified and mitigated in a CDC clearance process. And the web content was not updated on Thursday to reflect the change. So we need greater clarity on how the decision was made, what evidence was considered and who was involved in making it. But this policy roll out doesn’t smell, look or feel like CDC’s culture. It could be a communications faux pas. This is at least the third instance where Dr. Walensky has had to walk back her comments and the Biden Administration has had to do damage control. First it was the muddled messaging on school reopening guidance in February. Then in April, it was a prelude to what happened Thursday - a confusing statement on whether vaccinated people could get infected or transmit to others before we had sufficient evidence to say either way and relatively few people were vaccinated. Patience is growing thin for poor public health communication.
I really, really wish this had been something communicated with a goal date in order to give people throughout society time to plan. Children 12+ just became eligible this week. Eligibility to all adults only began last month and many who got vaccinated on the first day of eligibility may still be waiting for their second dose. The President had already set a goal of July 4th to have 70% of Americans at least partially vaccinated. The Director could have said something like, “as long as things continue to go well, we anticipate that mask guidance will change on July 4th.” This likely would have inspired more people to get vaccinated than lifting the mask guidance. Look at how many people are still in the ASAP crowd when it comes to vaccine intention. As much as a third of unvaccinated Hispanic adults, 17% of Black adults and 16% of White adults. These are people who want to be vaccinated but have had barriers to access. I’d be curious to see how many of the Wait and See folks move into the ASAP camp after the mask guidance change. I hope Kaiser Family Foundation asks those who move to ASAP whether it was because of the incentive that they’d no longer need to wear a mask (the CDC Director’s gamble) or because they perceived that their risk just went up as fewer people were wearing masks.
Here’s my bigger fear though, and another predictable consequence. When a governor or other leader is deciding what to do with remaining CARES Act funding or new money coming from the federal government intended for vaccinations and facing the daunting task of inefficient and costly community-oriented vaccination, the new guidance might give them pause. When the CDC Director says that people have had the chance to get vaccinated, their health is in their own hands, and we are moving on, does the leader with vaccine money use that money to address vaccine access barriers and racial inequities? Or divert the money for other causes, eager to move on from the nightmare that was 2020 in their administration? And what if that leader is heading into an election year? My fear is that the policy roll out in this case, although it may have been intended to increase vaccination rates, will actually make it harder for the most vulnerable to access the vaccines. The decision ignored the reality of inequities in vaccination rates. Every person we vaccinate matters. But we are vaccinating fewer of the most vulnerable, and these are the people who need the vaccine the most. The areas with the highest death rates have the lowest vaccination rates. The people without health insurance are the least likely to be vaccinated. The poor are the least likely to be vaccinated. These communities are vulnerable and are often the hardest to reach.
For those who haven’t been vaccinated, with people unmasking in their community even though they’re also not vaccinated, the risk just went up in a big way. I wish that I had advance warning on this so that I could have gotten one last haircut for my kids. We’re no longer taking them to the store, even masked. Each family is back to having to calculate their own risk tolerance in a shifting landscape where it is harder to identify what or who those risks are. People who are immunocompromised feel forgotten. It feels like whatever led to this decision, it was rushed and not well thought out and a lot of people feel let down. There’s chatter that CDC will provide clearer guidance this week for schools and businesses. But it’s hard to put toothpaste back in the tube. In public health every word matters. The stakes are high. The wrong words were chosen here. We’ll have to see what the impact the words have in terms of cases, hospitalizations and deaths.
References
https://dph.georgia.gov/covid-19-daily-status-report
https://covid-gagio.hub.arcgis.com/
https://www.kff.org/coronavirus-covid-19/dashboard/kff-covid-19-vaccine-monitor-dashboard/
https://www.kff.org/coronavirus-covid-19/issue-brief/vaccination-is-local-covid-19-vaccination-rates-vary-by-county-and-key-characteristics/
Georgia COVID-19 Updates is a free newsletter that depends on reader support. If you wish to subscribe please click the link below. There are free and paid options available.
My Ph.D. is in Medical Microbiology and Immunology. I've worked at places like Creighton University, the Centers for Disease Control & Prevention and Mercer University School of Medicine. All thoughts are my professional opinion and should not be considered medical advice.