The Week in Review, 26Dec - 03Jan2021
Georgia COVID-19 Updates
Happy Sunday! If you are someone who gathered outside of your household for New Years Eve, please consider yourself to be infected and quarantine for the 14 days that follow. The ideal range to seek a test after a high risk exposure is 4-7 days after the event, so Tuesday through Friday of this week. Even if your test is negative, the safest thing to do is to quarantine the full length of time. Because a negative test only means that you were negative on the date when your specimen was collected. It’s possible that you could truly be infected but too early in your disease process for the virus to be detected.
For my readers over the age of 65 or who have underlying medical conditions, it is really unsafe for you to be indoors with anyone from outside of your immediate household right now, especially if masks are not being worn. It is a good time to shelter in place as much as possible and have your groceries and/or medications delivered. The people who gathered for New Years Eve are going to be infectious this week and may be out in public.
Combined Data
Let’s begin with a look at how three of our main metrics are trending over time. The graph below lets us see all three together, with cases (blue line) corresponding to the left y-axis and hospitalizations and deaths (gray and red lines, respectively) corresponding to the right y-axis.
This week we saw a big jump in cases. We also saw an increase in hospitalizations compared to last week, but it’s hard to know whether last week’s decrease was due to holiday reporting delays. We also saw a decrease in deaths. Again, we are still probably seeing some delays in reporting due to the holidays.
Testing
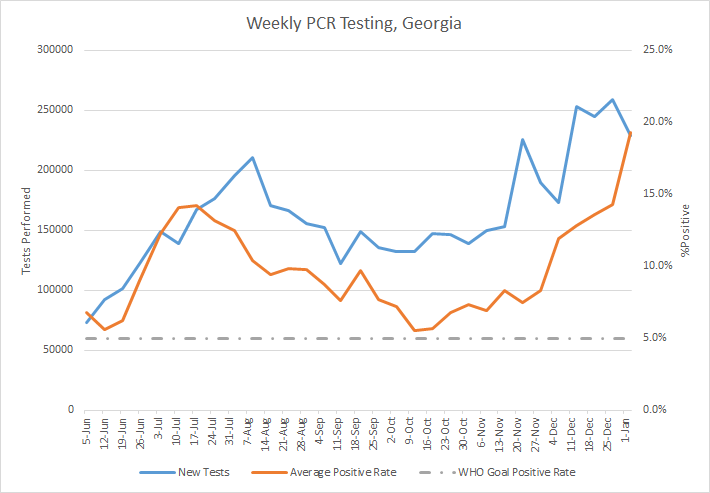
Today was a mid-range PCR test output day (25,253) and 20.8% of those tests were positive, or one in five. For the week, there were 228,713 PCR tests reported, a decrease of 11.8% compared to the previous week. Of all of this week’s PCR tests, 19.3% were positive. It’s the highest weekly positive rate that I’ve recorded since early June. The percent positive rate has increased by 132.5% since Thanksgiving.
There is not a single county in Georgia that is at or below 5% for test positivity over the past two weeks. The lowest percent positive rate is for Wilcox county in southcentral Georgia, at 6.6%.
Having a high positive rate is an indication that we aren’t testing widely enough and are missing cases. So as big as our case numbers are, we are missing a lot of cases and there is probably a lot more disease out there than we realize.
The Georgia Department of Public Health does not provide any data on antigen testing, but we know that antigen testing identified 15,232 of the 58,601 cases this week (or 26%). So there is a lot of information we don’t get to see.
Cases
The number of combined new cases (by date of report) is as follows:
- 24 hours: 5077 by PCR + 701 by antigen = 5778 (+0.8%)
- 7 days: 43,369 by PCR + 15,232 by antigen = 58,601 (+9.3%)
- 4 weeks: 143,254 by PCR + 46,241 by antigen = 189,495 (+37.8%)
The new statewide total is 690,900, combining PCR and antigen-test identified cases. We will probably cross 700,000 by Tuesday. Bear in mind that these case totals are likely an under count of our actual case count - it’s a problem that plagues public health for multiple diseases and especially so when a disease has so many asymptomatic cases, as COVID-19 does. But also because we know that our percent positive rate is high. Our number of cases have grown nearly 38% in the past month and of all the cases that have been recorded in Georgia to date, 27.4% were reported in the past 4 weeks. In other words, more than one in four of the cases we’ve had so far were in the last month, even as we are in the 10th month of this pandemic. In the graph below, I show the Georgia cases by date of report for both PCR and antigen cases for each county type. Ignore the big bump around 11Oct - that was a data dump of antigen cases. You’ll notice that we are well above the previous summer surge now. In fact, our 7-day rolling average is now 141% higher than our previous peak. But the Atlanta counties (Fulton and DeKalb, blue line) are faring better than other county types in the state. Rural counties have the highest 7-day case rate in the state.
The Georgia DPH does not provide demographic data on any of its antigen positive cases, despite the fact that they account for 26% of this week’s cases. The graph shows what we know about age groups based on PCR cases alone. You’re looking at 8 week timelines for each age group, side by side. We saw increases in every age group other than children 0-17. Cases are >200% higher now than 8 weeks ago for all age groups over 30 and infants under the age of 1. Young adults, aged 18-29 remain our single biggest contributor to cases but really everyone between 18 - 59 is playing an important role in how this pandemic grows.
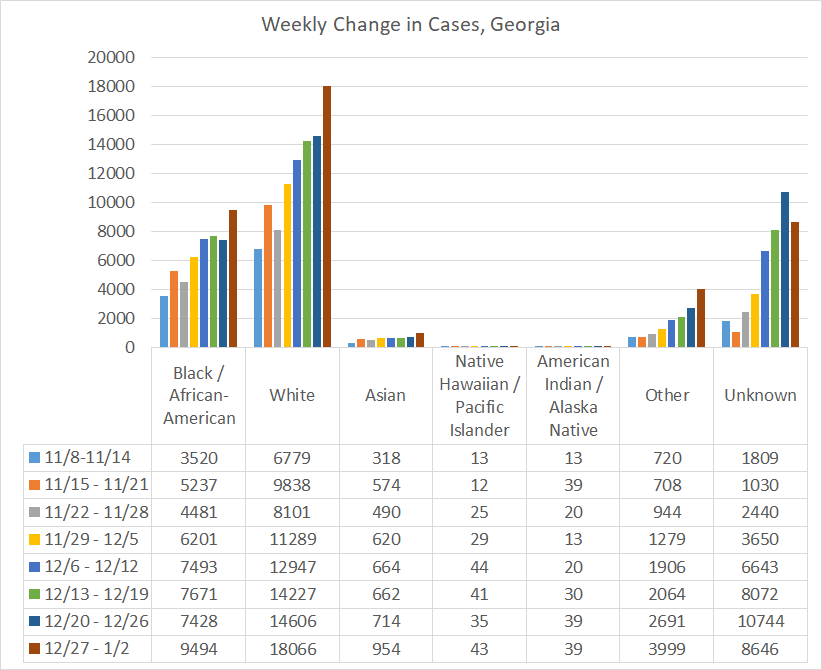
If we look at the demographic breakdown of cases by race, we see some concerning trends. First, this week we saw a 49% increase in cases among the “other” category (contains the majority of people who identify as Hispanic), 37% increase among Asians, and 28% increase among Black / African-American populations. Despite the fact that this graph shows White populations as the biggest contributor to cases (and they are, partly due to their makeup of the overall population) their weekly increase was comparatively less than for people of color (+24%).
The other thing that’s really concerning, is how much cases have grown in the “unknown” category. This is a holding area for cases until contact tracers are able to gain more information. Eventually they get sorted into their proper categories. Seeing this category grow as it is for race and also age is an indication that those who collect these data are getting overwhelmed by the influx of cases. That has important ramifications beyond demographic data collection. If they aren’t able to contact and collect this information, they likely aren’t able to perform contact tracing either. When contact tracers get overwhelmed, that means we have a weakened ability to limit disease transmission and find sick individuals. Meanwhile, this disease burns through our communities.
Hospitalizations
The number of hospital and ICU admissions for COVID-19 (by date of report) is as follows:
- 24 hours: 56 admissions, 9 admissions to the ICU
- 7 days: 1696 admissions, 230 admissions to the ICU
- 4 weeks: 6444 admissions, 790 admissions to ICU
The number of COVID-19 patients currently in the hospital is 4921 and their proportion of the total population of hospitalized patients (called the COVID-19 patient census) is 30.5%. So almost one in three patients hospitalized in Georgia are there because of COVID-19. The number of patients currently admitted is 20% higher than we saw last week on Sunday. Of course, the COVID-19 patient census varies by region, with some areas experiencing COVID-19 more acutely than others. The areas with the highest COVID-19 patient census (compared to all hospitalized patients) are regions M (44.2%), A (42.5%), and E (41.6%), see the far right column in the graphic below. Today Region J (coastal Georgia) joined the rest of the state and is now in the dark red zone.
One of the most critical resources in the treatment and management of the most severe cases of COVID-19 is ICU bed space and ventilators. Today, 89.8% of the state’s ICU beds are full. As of yesterday’s HHS Community Profile Report, 41% of those beds are held by a COVID-19 patient, nearing half of all ICU beds in use. Thankfully, no hospital region in Georgia is maxed out for ICU bed space today, but 10 of the 14 hospital regions are using >90% of their beds. This means there are fewer beds available for critically ill patients, including people who have heart attacks and strokes, car accidents, etc. Forty one percent of the adult ventilators across the state are in use and the HHS report indicates that 14% of the ventilators are in use by a COVID-19 patient. We have been getting warnings for weeks now that our hospitals are getting overwhelmed. We see it in the data too. But unlike during the summer surge when these reports were enough to compel people to take the disease seriously and limit transmission, that doesn’t appear to be happening this time. Or at least, not yet in any way that we can see in the data. It is critically important that we do what we can to flatten the curve now to avoid rationing of care and to preserve healthcare capacity.
This week we saw an increase in hospital admissions for most age groups (except those 0-4). Over the past 8 weeks, the increases have been greatest among those 50-59 (+151%), 80+ (+146%), and 30-39 (+144%).
If we look more closely at the ICU admissions over the past 8 weeks, by race, then we see that the largest increases are among White populations (+95%). The next highest increase is among Black/African-American populations, at +35%.
Of those who enter the hospital, 17.6% will require an ICU bed. Of those who require an ICU bed for COVID-19, the fatality rate is 37.4%. You avoid needing an ICU by limiting transmission in the first place.
Deaths
The number of new confirmed deaths (by date of report) is as follows. The percentage in parentheses indicates how the increase compares to Georgia’s cumulative total at the start of each window of time.
- 24 hours: 2 (+0.02%), death reporting is always low on the weekends.
- 7 days: 179 (+1.8%)
- 4 weeks: 922 (+10.3%)
This week the number of deaths decreased 35% compared to last week. However, it’s unclear how much of this might be due to delays in reporting with back to back holidays. I certainly hope that decline in deaths is real and that it continues. But I think it’s too early yet to know. The current statewide total of confirmed deaths is 9893 and of those, 9.3% were reported in the last 4 weeks alone.
The only age categories that saw an increase were 5-9 year olds and 30-39 year olds.
The table below shows us how many cases, hospitalizations and deaths have occurred among PCR cases. The top area shows the raw numbers and the hospitalization rate (of all cases, how many were hospitalized) and the case fatality rate (CFR, of all cases, how many have died). The bottom, colored in section shows aggregated information for children, younger adults and seniors. Proportion of cases/hospitalizations/deaths tells you how cases (etc.) among that age group compare to the total number of cases (etc.).
Some interesting things to note from this chart:
Both the hospitalization rate and the case fatality rate increase with age.
Although seniors make up just 19.2% of the PCR cases since the start of the pandemic, they make up 85% of the deaths and 53% of the hospitalizations. Their death rate is 18 times higher than that of younger adults. One in five seniors who get infected will be sick enough to need a hospital admission. If you break it down into the 10-year age cohorts, one in three seniors >80 years of age will need a hospital admission.
While we tend to think of the younger adults (18 - 59) as more invincible to the virus’s most devastating effects, they still make up 45% of all the hospital admissions recorded so far.
That’s it for now. Enjoy the rest of your weekend!
References
https://dph.georgia.gov/covid-19-daily-status-report
https://covid-gagio.hub.arcgis.com/
https://beta.healthdata.gov/National/COVID-19-Community-Profile-Report/gqxm-d9w9
Georgia COVID-19 Updates is a free newsletter that depends on reader support. If you wish to subscribe please click the link below. There are free and paid options available.
My Ph.D. is in Medical Microbiology and Immunology. I've worked at places like Creighton University, the Centers for Disease Control & Prevention and Mercer University School of Medicine. All thoughts are my professional opinion and should not be considered medical advice.