The Week in Review, 18 - 24Jan2021
Georgia COVID-19 Updates
Combined Data
The graph below shows how four of our big metrics for tracking the COVID-19 pandemic are tracking over time. Cases are represented by the blue line and correspond with the left y-axis. All other metrics correspond with the right y-axis. The reason I graph all of these things together is so that we can see the way these things trend together (or differently) over time.
This week we are continuing to see cases and hospital admissions decline for COVID-19 and they are doing this at the same time. That’s roughly consistent with what we observed during the summer surge. In the summer, these two peaks were a week apart, but this time they’re happening at the same time. However, what stands apart this time around is that the winter case peak was 152% higher than the summer peak, whereas the winter hospital admissions peak was nearly equivalent to the summer peak. ICU admissions (yellow) haven’t seen the big spike and fall that was observed in the summer. Instead, the increase has been more gradual and ICU admissions don’t appear to be dropping off as fast as general hospital admissions.
However, the same cannot be said for deaths. There wasn’t a massive jump in deaths this week, but they remain high. Also, it’s not clear that we have peaked yet. In the past, deaths peaked 2-3 weeks after cases and hospitalizations. So we may still have at least one more week of high death numbers to go. In the meantime, even at this point, the weekly death total is 53% higher than the peak we experienced in the summer.
Testing
This week we set a record for PCR tests performed in a single week, at 283,419. Of those, 14.7% were positive. The test output trend over time can be seen in the graph below, represented by the blue line that corresponds with the left y-axis. The red line represents the test positivity rate over time, and corresponds with the right y-axis. The gray dashed line is the goal line for test positivity.
A common piece of misinformation you’ve no doubt heard is that “the reason we’re seeing more cases is because we’re doing more testing.” That has been pretty widely debunked since often we see case increases when testing decreases. However the inverse is also untrue. There has been a lot of speculation that testing would decrease as public health departments shifted focus and resources away from testing in favor of vaccinations and that this would artificially decrease the number of cases. But this week we saw PCR tests increase 12% compared to the previous week. During that same time, cases decreased 13.6%. So the decrease in cases cannot be explained by a decrease in testing, because testing actually increased during that time.
The Georgia Department of Public Health does not provide data regarding the number of antigen tests that have been performed nor how many were positive. Further, they do not provide any demographic details for cases identified by the antigen test. Keep that in mind as we go through the demographic data in the following sections. You’re only seeing part of the data. Meanwhile, antigen testing identified 25% of the cases this week.
Cases
The number of combined new cases (by date of report) is as follows:
- 24 hours: 4210 by PCR + 543 by antigen = 4753 (+0.6%)
- 7 days: 38,154 by PCR + 12,762 by antigen = 50,916 (+6.2%)
- 4 weeks: 174,825 by PCR + 59,787 by antigen = 234,612 (+37.1%)
Some good news is that we haven’t seen a daily case total this low since 28Dec. Some of this is due to weekend effect - with decreased reporting over the weekends. But even the weekends have had high reporting over the past few weeks. The new statewide total is 866,911, combining PCR and antigen-test identified cases. Bear in mind that as large as these case totals are, they are likely an under count of our actual case count - it’s a problem that plagues public health for multiple diseases and especially so when a disease has so many asymptomatic cases, as COVID-19 does. But also because we know that our percent positive rate is high. In the graph below, I show the Georgia cases by date of report for both PCR and antigen cases for each county type. Ignore the big bump around 11Oct - that was a data dump of antigen cases.
You’ll notice that we are well above the previous summer surge, but there’s a decrease from a peak two weeks ago. There’s a small increase for all county types except for Atlanta (Fulton and DeKalb counties) in the past few days. You’ll notice that the descent from the summer peak was not a straight line down. So it’s not unusual to see some variation in this descent. Hopefully that’s all this uptick is. For now, our 7-day rolling average is twice as high as the summer peak. So just keep in mind that our work isn’t finished here just because the case rate is declining. When you have this much disease, it’s very easy for momentum to turn and for new surges to begin. We need to continue to be aggressive in limiting disease transmission, going back to at least the pre-winter surge level, and ideally down to the pre-summer surge level if we can. The Atlanta counties (Fulton and DeKalb, blue line) are faring better than other county types in the state. Atlanta suburb counties have the highest 7-day case rate in the state.
I saw an article that indicated that cold medicine sales are down, due to the disease mitigation strategies we’re using against COVID-19. We also know that we are experiencing an extremely minimal influenza season this year. So just understand that the common cold is no longer common this year. If you start to experience cold or flu-like symptoms, it would be wise to seek a COVID-19 test.
The next two graphs show us some of the demographic details of those who are getting sick and testing positive. In each graph, you’re looking at 8-week timelines for each age group side by side.
This week we saw decreases in cases for every age group. Next, let’s look at how cases are trending based on race.
We saw decreases for most races this week, except American Indian / Alaska Native. But it’s very concerning that the second highest race category was for the “unknown” category. This is a holding spot for cases that are pending investigation. Seeing this category rise as it has in the past 8 weeks is an indication that the weekly case totals are exceeding the capacity of the contact tracing workforce. That makes it harder to notify, test and isolate the close contacts of known cases.
Hospitalizations
The number of combined new hospital admissions (by date of report) is as follows:
- 24 hours: 115 new COVID-19 admissions, 16 admissions to the ICU (weekend reporting is typically light)
- 7 days: 1766 new COVID-19 admissions, 242 ICU admissions
- 4 weeks: 7598 new COVID-19 admissions, 963 ICU admissions
As indicated above, reporting over the weekend is often less than we see during the week. However, today’s ICU admission rate is higher than we typically see on a Sunday. Today there are 4959 COVID-19 patients currently hospitalized, a decrease of 10% compared to the previous week. In fact, we haven’t seen this metric under 5000 since 03Jan. This metric has plateaued and decreased over the past two weeks. So it’s another good sign of progress, taken together with other hospital metrics.
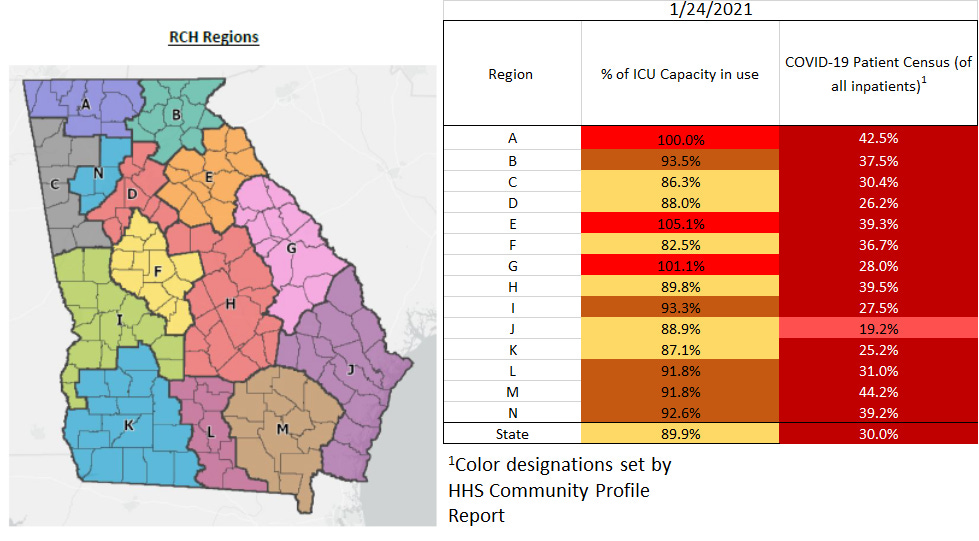
The graphic below shows us the Georgia Emergency Management Agency hospital regions. The table on the right tells you how each region is doing with respect to usage of their available ICU beds and how their COVID-19 patient population compares to their overall patient population.
There are some good signs here, even though we see so much red in the chart. First, there are only 3 regions that are maxed out for ICU beds, compared to 4 as we’ve seen recently. In addition, there are 6 regions now in the yellow zone (80-89.99%). In fact, the statewide average is now below 90% too. Let’s hope this trend continues in the coming week. All hospital regions continue to have a high COVID-19 patient census and all are in the red zone.
Next, let’s look at the demographic details that we have for hospitalizations.
This week we saw decreases for most age groups. The exception was really young children, 0 - 4 years old.
Deaths
The number of new confirmed deaths (by date of report) is as follows. The percentage in parentheses indicates how the increase compares to Georgia’s cumulative total at the start of each window of time.
- 24 hours: 3 (+0.3%)
- 7 days: 769 (+7%)
- 4 weeks: 2087 (+21.5%)
This week the number of deaths increased only 2.5% compared to the previous week. The current statewide total of confirmed deaths is 11,801 and of those, 17.7% were reported in the last 4 weeks alone. Of this week’s 769 newly reported deaths, 34% each came from rural and nonrural counties outside of the Atlanta metro. Another 21% came from Atlanta suburb counties and 9% came from the Atlanta counties of Fulton and DeKalb. The graph below shows how the 7-day death rate per 100,000 residents has trended over time for each county type. The state death rate is 49% above the peak during the summer surge. The death rate is worst for rural counties and best for the Atlanta counties of Fulton and DeKalb. In fact, the death rate in rural counties is 187% higher than the death rate in Atlanta.
Next, let’s look at the demographic data for this week’s deaths. Mercifully, deaths actually decreased for those 80+, although they remain very high. We saw increases for those aged 40-79.
Next, let’s see where this week’s newly reported deaths came from in terms of race. White and Asian populations saw a decrease this week, but there were increases for Black and “Other” race (the majority of Hispanic individuals are in this category).
It’s good to see some positive trends in the data. The emergence of the UK variant in the US is a serious concern, however, with a transmissibility rate that is estimated to be >40% higher than the wild type version of the SARS-CoV-2 virus we’ve been dealing with up to this time. It doesn’t appear to cause more severe disease so far. But with a higher transmissibility rate, that’s more “shots on goal” so to speak, for the virus. It will result in more hospitalizations and more deaths if it is able to take off in the United States. For this reason, limiting disease transmission is even more important now more than ever. It also makes contact tracing incredibly important, even as we see signs in the data that they’re overwhelmed. I really can’t think of a solid reason why anyone should be indoors with people they don’t live with while not wearing a mask other than dental procedures, etc. Of course, masks aren’t the only mitigation strategy we should be using, because none of them are perfect on their own. Instead, we need to layer them together. That’s why there are so many things you need to be concerned about all at once such as wearing a mask, keeping your distance from others, prioritizing outdoor interactions, observing good cough and hand hygiene, and getting the vaccine when it is made available to you.
That’s it for this week. I’ll be back tomorrow to put the Georgia pandemic in the national and global context.
References
https://dph.georgia.gov/covid-19-daily-status-report
https://covid-gagio.hub.arcgis.com/
https://www.bloomberg.com/news/articles/2021-01-21/more-masks-means-fewer-germs-hitting-p-g-s-cold-medicine-sales
Georgia COVID-19 Updates is a free newsletter that depends on reader support. If you wish to subscribe please click the link below. There are free and paid options available.
My Ph.D. is in Medical Microbiology and Immunology. I've worked at places like Creighton University, the Centers for Disease Control & Prevention and Mercer University School of Medicine. All thoughts are my professional opinion and should not be considered medical advice.










Thank you for your continued sharing of knowledge & expertise regarding this virus and it’s variants. Really appreciate being able to trust your numbers, graphs, charts etc. You are a trusted source for myself, family & friends as this pandemic continues to rage on.