The Daily Digest, 24Feb2021
Georgia COVID-19 Updates
Vaccine Update
There’s a lot of good news today. A LOT of good news. I’m scheduled to do vaccine Q&A on Friday and likely still will, but we just got the data today for the Johnson and Johnson COVID-19 vaccine clinical trials. As you may recall, there is a meeting on Friday for the Vaccines and Related Biological Products Advisory Committee (external to FDA) to consider recommending the J&J vaccine for Emergency Use Authorization. So I want to share a bit of the news we see from the clinical trial data today and may expand on Friday.
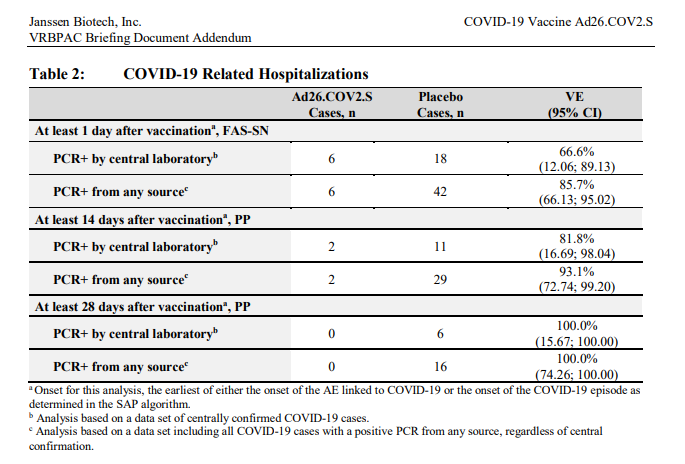
So far, it appears that the J&J vaccine isn’t as good as the Pfizer and Moderna vaccines at preventing cases. This isn’t necessarily new information. We had a heads up on this from the press release earlier this month. However, they are just as good at preventing hospitalizations (serious cases of COVID-19) and deaths. Let’s take a look at the table below. For whatever reason, here they distinguished between cases that were identified by PCR at their central laboratory versus any laboratory (i.e. people who went to their doctor or health department for testing). Let’s ignore the first line for each section (PCR+ by central laboratory) and look at the more inclusive data set (from any source). As early as 14 days, the vaccine showed efficacy against COVID-19 hospitalization at 93.1% and at least 28 days after vaccination, the efficacy was 100%.
So more people might get infected following vaccination than those vaccinated with the Pfizer and Moderna vaccines, but their infections are far more mild than what the placebo group experienced. Remember, COVID-19 infections are mild for most people in this pandemic even without the vaccine. But there are people for whom it is far more intense, including previously healthy people. I think it’s a significant goal to make the infection (if it happens at all) mild for EVERYONE. Eventually, as case rates drop in our communities, then there would be even fewer infections for those vaccinated with the J&J vaccine. And if the only cases that happen are mild, then this becomes a much more manageable situation from a community stand point. We don’t disrupt society due to the common cold. If we can bring COVID-19 down to common cold severity, then a return to “normal” is a lot more attainable. The bottom line to me is that there is no need to shop around for the “best” vaccine. Please just get the first one that is made available to you.
The Advisory Committee on Immunization Practices is meeting today and tomorrow too, but it doesn’t look like they’re planning to discuss COVID-19 this month. Instead, they’re focusing on other vaccines such as those for rabies, Dengue, tickborne encephalitis, hepatitis, Ebola, etc. It’s a good reminder that public health and infectious disease are more than just COVID-19. I anticipate that the ACIP will probably meet again, shortly after the FDA advisory panel makes a recommendation for EUA for the J&J vaccine. If and when that happens, I’ll be sure to share the highlights from that meeting.
A second piece of really, really good news is that we’re starting to see the earliest impact of the COVID-19 vaccines. As you may recall, they were prioritized first for healthcare workers and residents of long term care facilities (LTCFs). As of 24Nov2020, LTCF residents accounted for 6% of the US cases but 40% of the US deaths from COVID-19. So I think it’s pretty easy for us to appreciate WHY they were prioritized for the first phase of vaccination. The graph below comes from the Kaiser Family Foundation. It tracks weekly COVID-19 deaths per week, for the overall US population and for the nursing home population. Vaccinations at nursing homes began 21Dec2020. And whereas the overall US population (minus the nursing home population) saw deaths increase 61% over the next seven weeks, they decreased 66% for those in nursing homes.
Because of how our country has prioritized WHO gets the vaccine first, this is the earliest place we might have expected to see the vaccine’s impact in the data. The goal was to prevent deaths in the group most disproportionately impacted. And the vaccine is accomplishing that goal, despite what was happening outside the LTCFs. Eventually, we should expect to see similar trends for other subpopulations.
While we’re on the subject of joy and hopeful news, I saw this article today that describes a hospital in Portland, Oregon, where they had zero COVID-19 patients in the ICU for the first time in a year. I want you to continue to follow the public health recommendations to the best of your ability. But things are very much looking up. We just need to see this through.
Yesterday, an interview I did with Georgia Public Broadcasting on talking to those who are hesitant about the vaccines was broadcast nationally on the NPR program, Here and Now. As a follow up, I will say that for as many stories as we hear about those who are nervous about the vaccines, I would argue that there are just as many stories (even if they aren’t reported) of people who are willing to go to extraordinary lengths to get the vaccine. For those who want the vaccine, they REALLY want it and see it as a matter of life and death - because it is. We need to do more to get vaccines to these people, recognizing that the hurdles we’re asking people to jump are unreasonable for the working poor and marginalized communities. Mass vaccine clinics are a GREAT strategy. But going forward we also need to be taking the vaccine to poultry plants, factories and places where people can’t social distance well but also have the hardest time getting time off to attend a mass vaccine clinic. We need to eventually go door to door to reach homebound senior citizens or those without transportation. We don’t have the vaccine supply to do this well yet. But with the EUA of the J&J vaccine we will have a critical tool to protect some of the people who are hardest to reach - both because of the single dose format and the easy storage conditions. The time to start thinking about how to accomplish these things is now. J&J did not take the Operation Warp Speed incentives and so they have not been mass producing their vaccine prior to EUA. As a result, we have time to think about how best to leverage this vital tool to do the most good. Georgia was caught flat-footed compared to states like West Virginia and Alaska in thinking through the logistical challenges of deploying a large-scale vaccination effort, as we’ve seen in the data but also the difficulty of scheduling and follow up. Let’s hope that Georgia can be a LEADER with the J&J vaccine when it starts to arrive. It is my hope that Georgia can do better at partnering with local non-profits and community organizations, churches, etc, to bring the vaccine to those who are disproportionately impacted by deaths in this pandemic including rural and medically under served communities. Because the way vaccination efforts are currently structured favors those who are well off and well connected, who have the time, economic security, and internet savvy to manage a cumbersome appointment system, make hundreds of calls in a day, or to take a day off from work to go to a mass vaccine site. Yes, things will be better with more supply. But we can’t just keep doing more of what we’re already doing. We can do better if we are proactive.
Testing
For the last couple days we’ve seen a drop in the number of new cases that are reported through Electronic Laboratory Reporting (ELR) for both PCR and antigen cases. What this means is there are a lot of cases that are being reported through phone, email, fax, but not through the usual data collection. Sometimes, these are the result of data dumps and cleaning. But they don’t come with the denominator (total tests performed) that is needed to calculate percent positivity. As a result, test positivity is not really a trustworthy metric for today or yesterday.
Today there was a net increase of 20,380 new PCR tests reported through ELR and 7.2% of them were positive. But of the newly reported PCR-identified cases, only 72% came through ELR. We’re missing test positivity data for 28% of today’s cases. For antigen testing, there were 16,637 newly reported antigen tests and 6.7% were positive. Only 84% of today’s newly reported antigen cases were reported through ELR. So be careful about pinning too much hope to the positivity rates today.
Cases
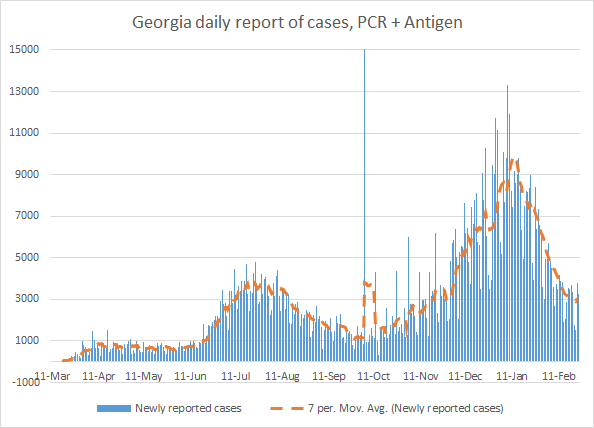
There were 2057 newly reported PCR cases and 1183 newly reported antigen cases today for a combined total of 3240 cases compared to yesterday’s total. In all, there have been 994,061 cases to date in Georgia.
I’m getting a little concerned that the 7-day case rate per 100,000 is starting to level out. Our descent from the winter surge has been both rapid and drastic, but it has slowed down. What we don’t want to happen is for this to be where we bottom out. Because at this point we are still 156% higher than the case rate where we entered the winter surge. That means that we have really high disease burden even as the more transmissible variant becomes dominant in Georgia, expected to happen in March.
The people who continue to ignore public health guidance now have a higher chance of catching and spreading this disease than before, because the new variant is 40-80% more transmissible. More cases means more hospitalizations and more deaths. Yes, we have prioritized vaccinating those over 65 who represent the majority of deaths. So it’s possible that the next surge won’t feature as many deaths as before and certainly not with the same age distribution. But it’s a shots on goal problem here. Those 65+ are a substantial part of the hospital burden, but there is significant hospitalization for younger age groups too. In fact, hospitalizations among 50-59 year olds are as great as those among 80+. The more cases we have, the more hospitalizations and the more deaths, even if they’re in younger age groups.
Georgia has never returned to pre-surge baseline in previous surges, however. It seems that with every surge the state just gets more comfortable with overburdened hospitals and deaths. But if this is where we’re bottoming out now then the race to vaccinate as many people as possible, as rapidly as possible, takes on new urgency.
Hospitalizations
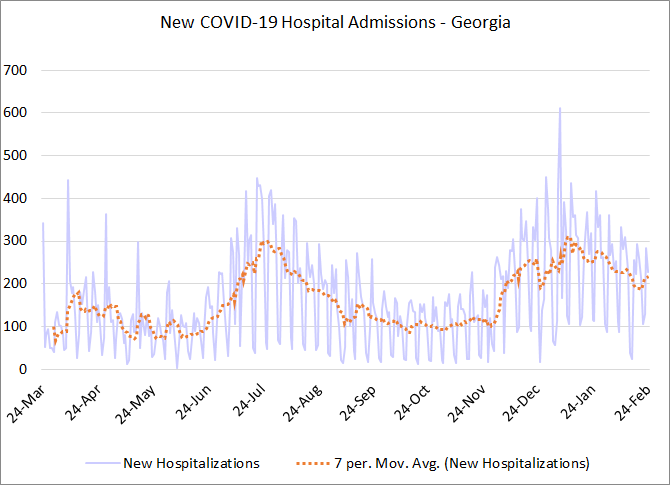
Today there was a net increase of 227 newly admitted COVID-19 patients and 32 patients were admitted to the ICU for COVID-19. You can see from the graph below that the daily admissions really haven’t declined very much from the winter surge peak, especially compared to what we saw following the summer surge. The daily hospitalization rate is more than twice as high as it was before the winter surge.
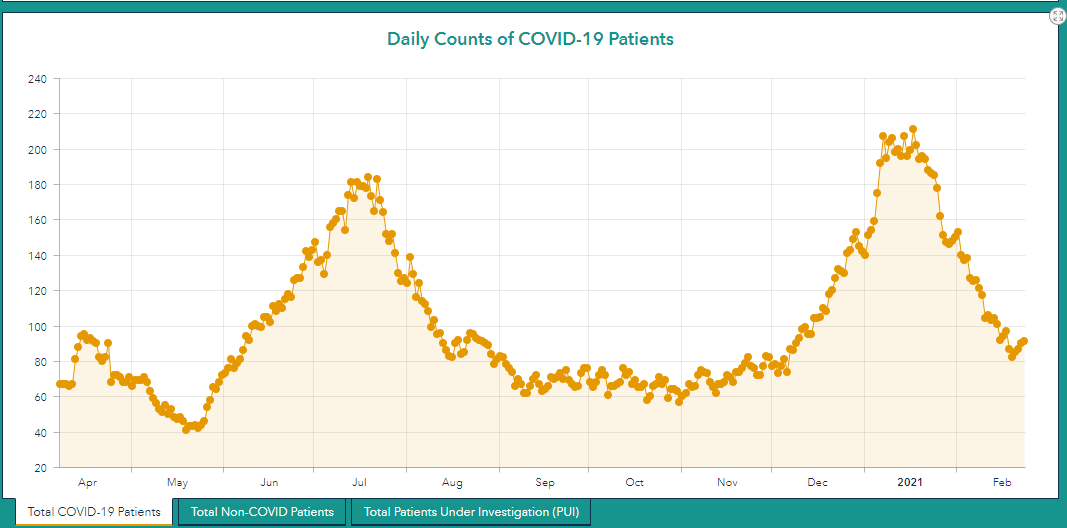
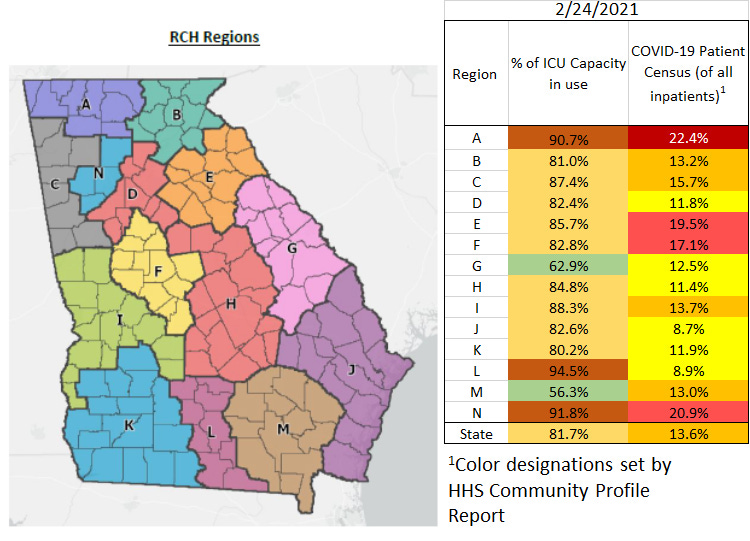
There are four regions where COVID-19 patient census (those with COVID-19 compared to all hospitalized patients) has decreased back to pre-winter surge levels. They are regions H, I, L and M. But there are 9 hospital regions (of 14) where the patient census number has leveled off in its descent as we are seeing for cases also (A, B, C, E, F, H, I, L and M). In fact, for two of them (regions A and I) we see that they have bottomed out and actually started to increase once again. The graph for region I is shown below, demonstrating the rebound in COVID-19 patient census.
It’s a little early yet to know if this is something to worry about. This rebound could be reversed in the coming days and this is just the new baseline. But it is concerning to see so many regions leveling off at once.
The graphic below shows where each region stands as of today with respect to ICU bed usage and COVID-19 patient census.
Deaths
It was unfortunately a high death reporting day, with 121 confirmed deaths and 16 probable deaths due to COVID-19. Yesterday there was a newly reported pediatric death, in a 14 year old girl from Gwinnett county. Hers is just one of 10 deaths in children under 18 since the start of the pandemic.
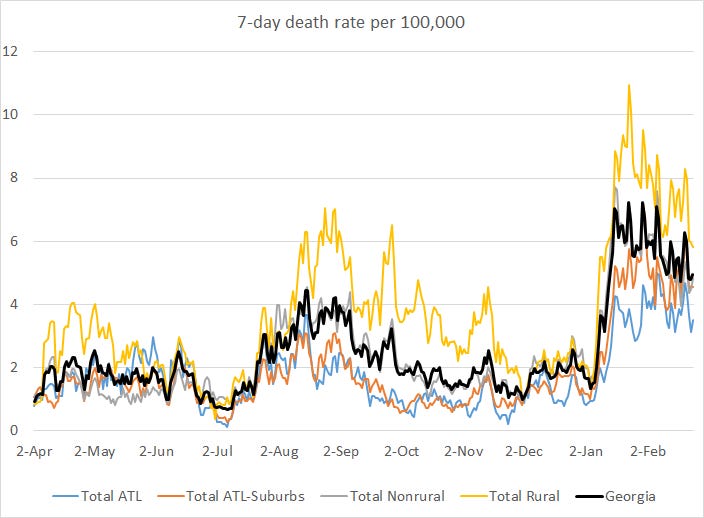
Of today’s newly reported deaths, 34% came from nonrural counties outside of the Atlanta metro and 26% came from rural counties. Atlanta counties (Fulton & DeKalb) and Atlanta suburb counties each contributed 18% of today’s newly reported deaths.
The death rate is starting to decline, but it is slow-going. The death rate at this point is about 4.5 times higher than it was when Georgia entered the winter surge.
So today’s newsletter is a mix of extreme optimism and hope about the vaccines mixed with some warning signs that we haven’t finished the job of bringing metrics down to pre-surge levels. If you’ve taken a break from the public health recommendations to properly wear a mask and social distance and avoid unnecessary errands, this would be a good time to resume doing so. Because the end is in sight and it would be a real shame to lose people unnecessarily when we are this close to having ample supply of vaccine. We just need to hold out a bit longer. Please do the work to make the winter surge the last one that Georgia experiences.
References
https://www.cdc.gov/vaccines/acip/meetings/slides-2021-2-24-25.html
https://www.fda.gov/advisory-committees/advisory-committee-calendar/vaccines-and-related-biological-products-advisory-committee-february-26-2021-meeting-announcement
https://www.fda.gov/media/146218/download
https://www.kff.org/policy-watch/is-the-end-of-the-long-term-care-crisis-within-sight-new-covid-19-cases-and-deaths-in-long-term-care-facilities-are-dropping/
https://www.13wmaz.com/article/news/health/coronavirus/providence-portland-no-covid-patients-critical-care/283-567aeac9-d874-4113-9923-959730aacb31?fbclid=IwAR15rUsFtrqcnsuFAkGWcnsbUSl-zza5DEbpriijMWxfgtHEC42FCp2UKRM
https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2020-12/COVID-02-Dooling.pdf
https://dph.georgia.gov/covid-19-daily-status-report
https://covid-gagio.hub.arcgis.com/
Georgia COVID-19 Updates is a free newsletter that depends on reader support. If you wish to subscribe please click the link below. There are free and paid options available.
My Ph.D. is in Medical Microbiology and Immunology. I've worked at places like Creighton University, the Centers for Disease Control & Prevention and Mercer University School of Medicine. All thoughts are my professional opinion and should not be considered medical advice.