Vaccine Update
Today we’re getting some new information on allergic reactions following vaccination with the Moderna vaccine. It appears that these allergic reactions are very, very rare. I should point out that while the risk of anaphylaxis is rare, this is the reason why you are asked to wait in the setting where you received any vaccine (not just COVID-19) for 15-30 minutes afterwards. Americans typically ignore that advice but it is still recommended. This is not a unique thing to to the COVID-19 vaccines.
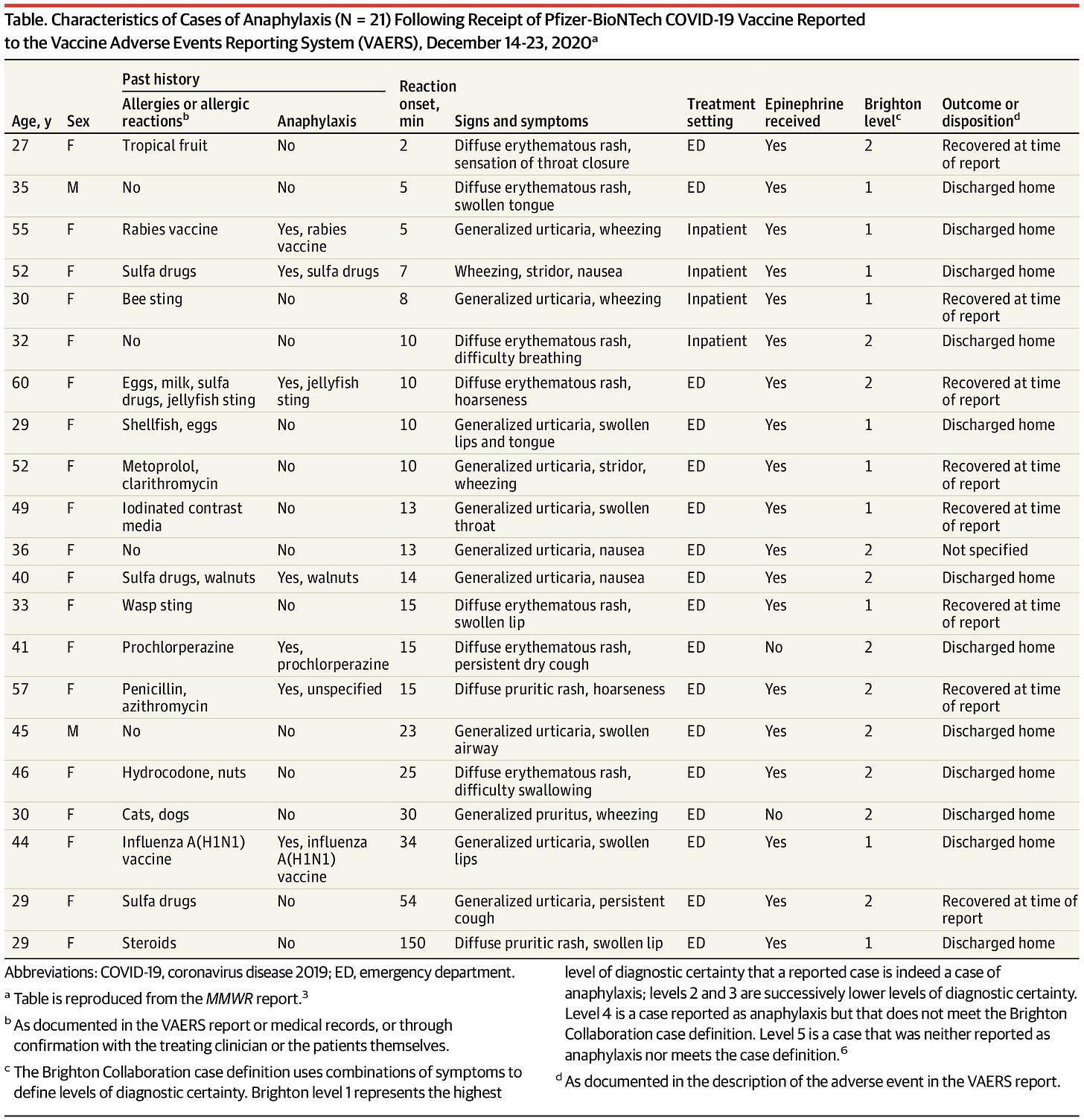
Here’s an early look the patients who experienced anaphylaxis in the first week of the Pfizer vaccine rollout. The columns on the left tell you some of the demographic details for each patient and their past history with allergies and anaphylaxis. Starting with the column labeled “reaction onset, min” we’re talking about the COVID-19 vaccine experience for all remaining columns to the right.
Starting with demographic details, you’ll notice that the majority of these cases were in women. There’s evidence that hypersensitivity reactions are more common in women than men, so that’s not shocking. Seven of the 21 patients in this case had previous experience with anaphylaxis. Among those 7, in at least four of them their trigger was medications or other vaccines. Next, let’s move to the reaction onset column. This indicates how long the interval was between when the vaccine was given and when they began experiencing symptoms. All but 3 of the patients had their symptoms begin within 30 minutes of the vaccine administration. The next column describes their symptoms and there are probably some new vocabulary terms here for you. Erythematous rash = red skin that looks like a sunburn. Generalized uticaria = hives. Stridor = severe difficulty breathing. Pruritic rash = itchy rash. All patients were treated either in an emergency department or they were already inpatients at a medical facility. All but 2 were treated with epinephrine (this is that the “epi” stands for in EpiPen). At least from this report, none experienced long term complications or death.
A similar report was released by the CDC today with respect to the Moderna vaccine. This was a longer span of time, probably due to the holidays. But there were fewer instances of anaphylaxis investigated during that time. All of the patients described were female. Half of them had a previous episode of anaphylaxis.
In addition, the Kaiser Family Foundation did a survey on how people are feeling about the vaccine rollout. There are lots of interesting things here about the political divide as well as confidence in the vaccine for people of color. But I want to point out something that pertains most to the work that I do here. The majority of people in their survey did not have enough information to know when and where they would be getting a vaccine. A big part of this is due to the shortage of vaccines and the 50 state effort at distribution, rather than a coordinated federal response. Hopefully we will see more coordination from the new Biden administration. But it was disproportionately worse for Black and Hispanic adults as well as those whose household income was <$40,000 per year.
We definitely have work to do to improve communications more broadly to improve confidence in the vaccine and get the word out about its safety and benefits. However, this survey also tell us that we will need a multi-cultural communications strategy to inform, educate and empower. So far the state of Georgia’s communications strategy for this vaccine is to ask those who are vaccinated to post their selfies and reasons for vaccinating. That will help, of course, because the people you know are often more effective messengers even than elected leaders and celebrities. But we need a coordinated effort with actual resources behind it (i.e. money and communications staff). It’s getting really tedious to see the state continually asking people to do things for free and then just rely on that to carry the message.
Public Health Advocacy
Last time I wrote to you I expressed my confusion and frustration over the Governor’s budget proposal for the Department of Public Health. I mean, if there was ever a time to increase funding for public health, it’s during a pandemic. Please reach out to your elected representatives in the Georgia Legislature if you haven’t already done so and express your demand for additional funding for DPH above and beyond the Governor’s proposal. You can look up your representation here. But in addition to those who represent you directly, we also need to be contacting the members of the House and Senate appropriations subcommittees that will make the actual budget recommendations for the legislature to vote on. The committee for the Georgia House is shown below and you can click on their names for contact info at this link.
The list of committee members in the Georgia Senate appropriations subcommittee on Human Development and Public Health for the current session are shown below. You can locate their contact information here.
Again, it is important to contact both your elected representatives as well as the appropriations subcommittees. It’s also important to identify yourself as their constituent by providing your mailing address, reminding them that you are a voter, and then indicate your expectations that they bolster public health funding. I’ll work on some talking points for the next newsletter, but some of you will already know what to do and say and just need to know who to contact. Thank you for your support of public health!
Testing
It was a robust day for testing, with 49,452 newly reported PCR test results. However, Georgia still lags behind the rest of the nation with turning tests around quickly. We are ranked #47 in the nation for getting test results within 3 days, at 71% of all RT-PCR tests performed. Of today’s newly reported PCR test results, 13.9% were positive. The graph below shows how test positivity has trended over time. It’s good to see the trend moving downward.
Cases
The School Aged Surveillance Data report has not yet been released for this week. It is due today. So unfortunately, I cannot discuss the data trends for pediatric populations today.
Today there was a net increase of 8374 newly reported cases (6442 by PCR, 1932 by antigen test) compared to the previous day. Of today’s newly reported cases, 37% came from nonrural counties outside of the Atlanta metro. Next was Atlanta suburb counties, contributing 31.4% of today’s cases, followed by rural counties (20.7%). The graph below shows the 7-day case rate per 100,000 residents over time for different county types across the state. The statewide average is shown in black.
Atlanta counties (blue line) have weathered this surge better than the rest of the state. What’s interesting is what’s going on with the descent right now. First, it’s a lot steeper than previous declines after a surge. Previously they were more flat at the top and more of a gradual decrease. Another thing that’s a little strange is that there is a big dichotomy between the Atlanta counties (best case rate) and the Atlanta suburbs (worst case rate). Whereas every other county type is essentially in free fall, the descent is more subtle or has even leveled off over the past couple days for the Atlanta suburb counties.
The map below is formatted in the same way as the Georgia DPH map as far as the color ramp break points, but includes antigen cases as well as the PCR ones. You can click on the map to see a live image where you can click/hover over your county of interest to see the numbers. There are 92 counties above the 930 mark (the top end of the color ramp).
Hospitalizations
Today there were 270 new admissions to the hospital for COVID-19 and 44 new admissions to the ICU. The graph on the left (below) shows the trend in hospital admissions over time, with significant noise in the data over the holidays. There are 5196 patients currently hospitalized for COVID-19 and you can observe that trend in the graph on the right. Like for cases, the dropoff from this surge peak is more rapid than what we observed during the summer surge.
There continues to be considerable strain for hospitals across the state. There are three regions (A, E, and G) that have been using an overage of their ICU beds. The HHS Community Profile Report for 20Jan2021 tells us that 48% of the state’s ICU beds are occupied by a COVID-19 patient. That’s more than half of the 91.1% of state ICU beds that are in use overall. Furthermore, 11 of the 14 hospital regions are using in excess of 90% of their ICU beds.
The second column in the chart tells us how many COVID-19 patients there are relative to all inpatients for a hospital region. These numbers have been declining over the past few days for most regions. But we did see an uptick today for region M.
Deaths
Unfortunately, I think we’re still in for a couple more weeks of big numbers when it comes to deaths. That’s because death surges follow case/hospital surges at a delay of about 2-3 weeks. So given that cases and hospitalizations appear to have crested last week, we might not expect deaths to peak for another 2 weeks or so. Today there was a net increase of 159 newly reported confirmed COVID-19 deaths. The death rate for the state per 100,000 residents is currently 36% higher than the peak we experienced in the summer.
In the graph above we can see that death rate is declining for nonrural counties and the Atlanta counties of Fulton and DeKalb. Meanwhile, things are sort of steady for Atlanta suburb counties. But what’s interesting, and tragic, is that the death rate continues to climb for rural counties. The 7-day death rate in rural Georgia is 156% higher than the current death rate in Atlanta.
There’s growing concern over the COVID-19 variants from the United Kingdom and from South Africa. These variants, or mutants, are the result of the naturally occurring, random mutations that occur in the viral genetic material every time it replicates. It replicates when it is transmitted to a new person. So the fact that we have uncontrolled disease in this state and country makes it more likely that mutations happen. A lot of the times, these mutations are silent - meaning that they don’t really change the shape or function of any of the viral proteins. But, on occasion, the mutations have a meaningful impact. The UK variant appears to be more transmissible, meaning that a person can infect more people than if they were infected with the main COVID-19 strain we’ve been focused on (also known as the wild type). So far, it doesn’t appear to not be covered by the vaccine or by the monoclonal antibody treatments we have. However, there is evidence to suggest that the variant coming from South Africa is different enough that it can escape the immunity provided by monoclonal antibodies (these are pre-made antibodies that can be used early in infection as a treatment). We don’t yet know what this means for the immunity provided by the vaccine. But what both variants tell us is that we need to do more to limit transmission through coordinated government interventions and by accelerating the pace of vaccinations. We also need the federal and state government to do more to detect these mutants as they’re occurring. Other nations are far more aggressive in performing genomic surveillance of these viral variants. But the US has lagged behind. Yesterday, Dr. Toomey indicated that they only screen a small subset of the samples they receive for these genetic variants. And you can’t find something if you’re not looking for it.
The good news is that we can limit the spread of these variants by limiting the transmission of COVID-19 overall and that will also limit the generation of additional variants. There is some concern that we may need better masks to protect us against the UK variant. I will add a personal note here to say that I have begun double masking in light of the UK variant, even though none have been detected in my local area. Knowing that our genomic surveillance is so poor in this country and how many variant cases have been identified in multiple states without history of recent travel, I assume it is already here. But considering how many people aren’t wearing masks at all (or improperly), getting people to wear any mask will be an important improvement at this point.
So please continue to keep up the good work of preventing disease transmission. I know this is tiresome and frustrating. But I appreciate your efforts nonetheless.
References
https://jamanetwork.com/journals/jama/fullarticle/2775646?guestAccessKey=1441aa96-9dc6-4d50-85f8-8dcbd270a551&utm_source=twitter&utm_medium=social_jama&utm_term=4423375686&utm_campaign=article_alert&linkId=109655085
https://www.cdc.gov/mmwr/volumes/70/wr/mm7004e1.htm?s_cid=mm7004e1_w
https://www.kff.org/coronavirus-covid-19/report/kff-covid-19-vaccine-monitor-january-2021/
Georgia COVID-19 Updates is a free newsletter that depends on reader support. If you wish to subscribe please click the link below. There are free and paid options available.
My Ph.D. is in Medical Microbiology and Immunology. I've worked at places like Creighton University, the Centers for Disease Control & Prevention and Mercer University School of Medicine. All thoughts are my professional opinion and should not be considered medical advice.