The Daily Digest, 21Aug2020
Georgia COVID-19 Updates
Good evening! I hope that everyone has a safe, socially distanced weekend. I’ll be back on Sunday with the week in review.
Testing
Today there were 23267 new PCR/Diagnostic tests reported by the Georgia Department of Public Health. Of those, 2398 were positive for a percent positive rate of 10.3%.
Here’s how total tests performed are trending. The red line is the 7-day moving average. The blue line is total counts. What you’ll notice is that we are seeing a decent decline compared to a week ago.

Cases
There was a net increase of 2889 cases with today’s report and that brings the statewide total to 249,630. We should expect to surpass 250,000 tomorrow. Of the new cases that were reported today, 28% of them were backdated prior to the 14-day window. This demonstrates the way that delays in test turnaround time and possible lab backlogs are making it challenging to see how the pandemic is unfolding. For comparison, the proportion of cases that were backdated prior to the 14-day window at the beginning of the June case surge was about 8%.
For today’s cases, 32.5% came from nonrural counties outside of the Atlanta metro. 29.3% came from the Atlanta suburbs. 24% came from rural counties and 15% came from the Atlanta counties of Fulton and DeKalb.
Hospitalizations
Current hospitalizations continue to decline. That’s a good thing, but I don’t think that hospitals are reporting the number of COVID patients they are managing through telemedicine (for more see the section at the end of today’s report). That’s one reason why we can’t rely on one metric of this pandemic alone. So I’m only cautiously optimistic about the decline in current hospitalizations because we don’t know the full context of what that number means right now. It will be interesting to see what comes with next week’s White House Coronavirus Task Force report, since they also include patients under investigation in their data.
There were 245 new hospital admissions today and the overall hospitalization rate since the start of the pandemic is now at 9.3%.
Deaths
Unfortunately, it was a big day for deaths with a net increase of 94 compared to yesterday’s totals. The new statewide total is 4998 and we should prepare to cross 5000 tomorrow. When graphed by date of death, our deaths continue to climb and we are well above our previous peak in late April - early May.

Of today’s deaths, 35 came from rural counties and another 34 came from nonrural counties outside of the Atlanta metro. In other words, 73.4% of today’s newly reported deaths came from outside the Atlanta metro. Below you can see how our deaths to date have been distributed by county type in the pie chart on the left. The line graph on the right shows us how we arrived at this point.

You can see that deaths are climbing at a steady increase that is steeper than for Atlanta or its suburbs. Nonrural deaths have overtaken rural ones but they remain close. So please don’t get complacent about this disease just because you live outside of the Atlanta metro. This isn’t just Atlanta’s problem. In fact, the problems are in many ways worse outside of Atlanta.
Lastly, I wanted to bring one other death metric to your attention and that is the case fatality rate (CFR). When cases began to surge in late June, they diluted the deaths and the CFR plummeted as a result. However, deaths followed the case surge, by about three weeks. And with the climbing death toll, the CFR stopped its descent.
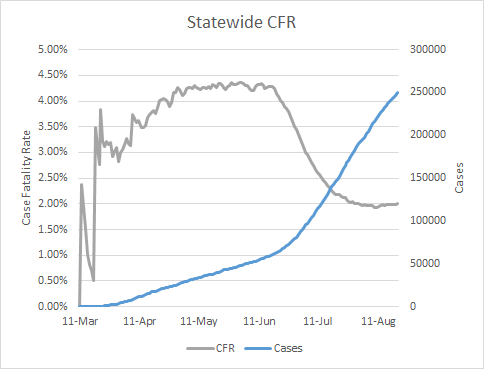
The CFR is starting to tick ever so slightly upward again. We climbed back to a CFR of 2% today and we haven’t seen the rate above 2% since August 1. This could be just the noise of day to day variation, but for us to see this small increase when our case surge has been so enormous means that there is significant momentum building in our deaths. Considering that our deaths by date of death graph shows an upward trend and no signs of slowing, I fear the CFR will also begin to climb. All COVID deaths have to start with an infection. So if we want to bring COVID deaths back down, we have to stop infections from happening in the first place. Please do all that you can to limit your exposures and the exposures you pose to others.
Something that I don’t know that we are appreciating fully is the toll this pandemic is taking on healthcare workers.
In the GEMA hospital bed capacity reports, most of tend to pay attention to how many beds are available for use (or unoccupied). But have you ever paid attention to how many beds are in their capacity in total? I’ve provided a graph showing how critical care bed capacity (total beds the hospital can support) have varied over time for hospital regions F and N, as an example. The data come from the GEMA daily reports. Beds don’t go away, but a critical care bed requires specialists to support the patient who occupies it. Fluctuations like we’re seeing below are a workforce problem. Perhaps the healthcare workers who support these beds have fallen ill or had vacation or other reasons for not being in the hospital. But the end result is that the bed is no longer supported for patient use.

Region F covers central Georgia and its critical care bed max capacity remained stable until hospitals surged starting in early July. But as healthcare workers get sick with COVID-19 and have to self-quarantine, they are sidelined from caring for the ill. That makes it difficult for our healthcare infrastructure to cope with strain. This is just the impact on critical care beds, but similar variation exists for other bed types too.
Current hospitalizations are on the decline and that’s great news. But part of it is the realization that we need to preserve bed capacity and the recognition that perhaps some of our COVID-19 patients can be carefully monitored at home if they have adequate monitoring devices and telemedicine. This is a triage strategy and it does not mean that the disease has gone away or is any less intense in our communities. However, because these patients aren’t admitted, it effectively takes people who would have been hospitalized under ordinary circumstances off the hospitalization tally. That this kind of triage is necessary should not be a celebration but a revelation of the ways that hospitals are preparing for the expectation that things will get worse. Applauding a decline in hospitalizations due to this artifact of the ways hospitals are triaging patients gives the impression that things are getting better and people will take more risks, thinking that things have gotten better in their communities. We should not aim to fill those hospitals again, even if the hospitals are preparing for that eventuality. So I think it’s important to see the broader context of what our decline in hospitalizations actually means.
Meanwhile, check out how infections among healthcare workers closely track the overall case curve for the state.

Effectively, when we get sick our healthcare workers get sick. And when they’re sick, they can’t work to care for the ill. As of yesterday’s DPH report, we have recorded 83 deaths among healthcare workers since the start of the pandemic. As DPH indicates in their disclaimer, this is likely an undercount since they don’t get profession data for each case and/or death. Furthermore, death and infection aren’t the only burdens on healthcare workers but also burnout, mental health stress and other challenges. Our healthcare workers are not an unlimited or renewable resource and we need to respect that in our actions to limit transmission in our communities.
References
https://dph.georgia.gov/covid-19-daily-status-report
https://gema.georgia.gov/document/document/sitrep-320-819/download
https://www.masslive.com/coronavirus/2020/08/covid-pushes-expansion-of-hospital-at-home-treatment.html
The Georgia COVID-19 Updates is a free newsletter that relies on reader support. If you would like to subscribe, please click the button below. Free and paid subscriptions are available.
