The Daily Digest, 20Jan2021
Georgia COVID-19 Updates
Good afternoon! I’d like to begin by sharing the keynote speech that I gave at the University of Georgia College of Public Health State of the Public’s Health Conference last week. My speech was a mix of personal narrative, a pep talk for the people working in public health, and a call to action to improve science communication to the public.
I’d also encourage you to visit the link to the conference to see the other speakers, including discussion of science communication to address vaccine hesitancy, health equity and racial justice and behavioral health especially in the context of the opioid crisis in Georgia. It was a tremendously well done conference.
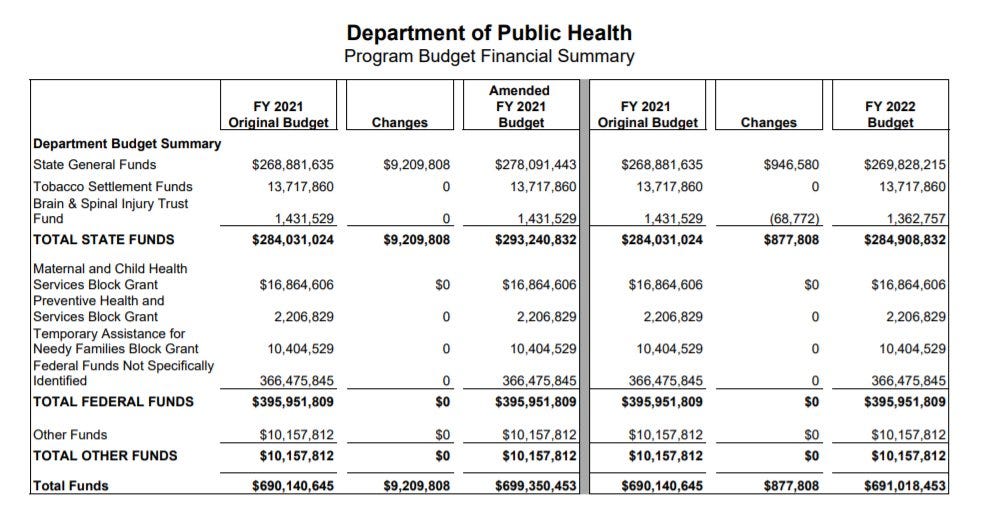
Something strange happened yesterday when Public Health Commissioner, Dr. Kathleen Toomey, presented the Governor’s budget proposal for DPH to the Georgia legislature. Despite the pandemic and the last decade of budget cuts to the Department of Public Health, the Governor asked for only a negligible increase in funding for Dr. Toomey’s department. This surprised me because every roadblock I’ve run across to improving the public health response to the pandemic has come down to money:
The state’s COVID-19 data task force was stood down in August because it ran out of money.
We can’t modify or add data visualizations to the dashboards because of money.
Vaccine rollout appear slow because of delayed reporting to the Georgia vaccine tracking system (GRITS) which has been described as “jurassic.” The system has been in place since the 1990s. Also, wouldn’t this be a great reason to bring back the state’s COVID-19 data task force? Again, we’re out of money.
We can’t add a centralized appointment system because of money.
You’ve seen the job announcements I’ve posted for DPH and everyone scoffs at the low pay for people with advanced degrees. We fix that with money.
You can see the full budget proposal here. The table below for the Department of Public Health can be seen on page 263 in the PDF.
Dr. Toomey went on to talk about how much the DPH was relying on volunteers to carry out testing and vaccinations. Over and over, the comments indicated how limited they were in terms of resources. And yet, she didn’t ask for additional funds. Furthermore, when asked about morale at the department and whether the public health professionals were getting additional pay during the pandemic, she replied that appreciation would matter more than money. That surprised me too, given the beleaguered accounts I’ve heard from public health professionals up and down the ranks about how they’re overworked, underfunded and understaffed. There are a lot of people working on COVID-19 even though respiratory disease isn’t their primary job function - people working on sexually transmitted diseases and other important issues have been reassigned to COVID-19. But rather than drop their primary job responsibility, they’re being asked to somehow manage both COVID-19 and their ordinary duties. That is an impossible ask for them to do both things well. I think at this point, bringing in reinforcements would help a lot. Money would allow them to bring in more reinforcements. I would also add that public health professionals do not go into this field to get rich - it is not a well-paying job or career field. And I can’t think of anyone more deserving of a raise in recognition of their service and dedication this year than public health professionals. I can imagine it is incredibly demoralizing to the public health workforce to know that help is not on the way. I’m incredibly sorry and the best that I can offer is to let you know how grateful I am for your service and that a good portion of the public is also grateful.
Instead, the Commissioner’s presentation indicated that the state’s pandemic response in its entirety would be funded solely by federal dollars. It signals that this pandemic is not Georgia’s problem and public health more broadly is not Georgia’s problem. This is despite being among the worst in the nation for infant and maternal mortality, getting children fully up to date on their vaccinations by age 3, the #1 state in the nation for new HIV cases and other public health metrics. These are efforts that are pushed to the side as the state copes with the pandemic but have been critically underfunded for at least the past decade. And seeing the perspective that public health isn’t a priority in the black and white of the Governor’s budget proposal helps to explain some of the deficiencies we’ve seen in the pandemic response and the vaccine rollout. It is deeply unfortunate, considering how many people have died, the strain experienced by public health professionals and healthcare workers and the way that all of our lives have been altered for so long. I can understand that no one in office today might have decided to run if they had known that 2020 would bring us a pandemic. No one dreams of governing through a pandemic. But it’s the reality we’re in and we need leadership to step up. I’d encourage you to reach out to your elected legislators now, as they are considering the state’s budget, to remind them that public health is a priority to you and increase funding for DPH above and beyond the Governor’s request. You can look up your representation here.
Here is a link to my notes from the presentation (see the speaker notes section) if you’d like to read them, including the Q&A from state legislators.
I’m getting a lot of emails from people so frustrated that they can’t find a vaccine appointment or to secure a testing appointment. The writers ask me to do something about it. I’m an advocate for public health and science communication, but I don’t work for the state of Georgia. I’ve served on the state’s COVID-19 data task force in a volunteer capacity, but that’s been stood down due to lack of funding. So I can offer my solidarity, but I can’t fix the appointment systems. I can share state resources, but I can’t fix them. My solidarity may offer comfort but it won’t get you to your goal, unfortunately. You may have more luck by reaching out to the Governor or the Public Health Commissioner. You can reach the Governor’s office here and Dr. Kathleen Toomey’s office here.
I have the most recent White House Coronavirus Task Force (WHCTF) report for the state of Georgia. You can review the document in full here. In the recommendations, Dr. Birx and colleagues say goodbye and thank their team and their state partners for their efforts. I’m not sure how these reports will take shape in the future. It would make sense to me that this responsibility would shift back to the Centers for Disease Control and Prevention. But we’ll see.
For vaccinations, the dose allocation per 100,000 residents for Georgia is higher than the national average, 9523 versus 9385. So Georgia is better off than many states. Georgia outpaced the nation for administration of the first vaccine dose over the past week (+72% compared to +58% nationally). It’s very encouraging to see Georgia improve in this way. However, we still remain behind the national average as far as first doses administered per 100,000 (1924 versus 3229 nationally). So we’re getting better but are still far behind. As far as people completing the 2-dose series, the WHCTF notes that 22,324 Georgians have done so as of 15Jan2021. That number is probably quite a big larger by now. It represents 0.3% of the adult population in Georgia. As of today, the CDC COVID Vaccine Tracker indicates Georgia remains #42 in the nation for first doses administered per 100,000 residents, moving up from #49.
Dr. Toomey and Governor Kemp have pointed out comparisons between states aren’t really fair because they have differently sized populations. That’s why looking at the data per 100,000 residents is so important - it corrects for population size differences. Using this correction, Georgia is ranked #42 - up from #49. They’ve also pointed out that the CDC COVID Vaccine Tracker doesn’t agree with the numbers that Georgia’s DPH tracker shows and they blame a disconnect in data transfer. But this is a problem presented to all 50 states and they’ve been able to overcome it. They further complain that the vaccine tracking system in Georgia (called GRITS) has been cumbersome for vaccine providers to use and fill out in real time. Yet, this is a problem also encountered by all 50 states. So I think we’re still waiting to hear a credible reason why Georgia is so far behind. As discussed above, I think we got a credible reason yesterday when we saw the administration’s budget priorities.
Testing
This week, the WHCTF noted an increase in tests performed per 100,000 for Georgia after a steep decline the week before. However, the Georgia test rate remains 49% below the national average. It is hard to find disease when you’re not looking for it, especially when cases are as high as they are.
The WHCTF also notes that the Georgia test positivity rate (18.4%) has decreased 14% compared to the previous week. However, it still remains 51% above the national positivity rate. It’s certainly good to see the positivity rate decreasing, but we are likely still missing a significant number of cases because we aren’t testing widely enough to find them.
Today, Georgia reported 44,460 new PCR test results, 13.4% of which were positive. That’s the lowest number we’ve seen since Christmas Day, certainly a good sign. Antigen testing identified 30% of today’s newly reported cases.
Cases
The WHCTF notes that Georgia’s case rate has slowed in its increase. More locally, we have noted a decrease in weekly cases, but we may be using different date cutoffs. According to the WHCTF, the Georgia case rate is 27% above the national rate. Of Georgia’s 159 counties, 151 are in the red zone, according to the WHCTF and four others are in the orange and yellow zones. This color classification is based on both case rate and test positivity rates.
Today Georgia reported a net increase of 5724 PCR-identified cases and 2481 antigen-identified cases for a combined total of 8205. That’s a high number but not unusual for the past two weeks. Of today’s newly reported cases, 33% came from nonrural counties outside of the Atlanta metro. Next was Atlanta suburb counties with 29% of today’s cases, 22% came from rural counties and 13% came from the Atlanta counties of Fulton and DeKalb.
What’s interesting about the decrease we’re seeing so far for this surge is how steep the descent is so far. This is a big departure from previous surges where the descent was more gradual. I’m not quite sure what to make of this yet, especially given that no statewide government interventions have been implemented. In any event, it is good to see the 7-day average drop the way that it is here. Hopefully that trend continues. At present, the case rate is greatest for Atlanta Suburb counties and best for the Atlanta counties of Fulton and DeKalb.
The top five counties for 14 day case rate per 100,000 residents are Madison, Warren, Taliaferro, Treutlen, and Wilkes. These are all rural counties. The counties with the lowest case rate per 100,000 are Long, Schley, Macon, Crawford, and Webster. These are also all rural counties.
Hospitalizations
Thankfully, the WHCTF notes that Georgia COVID-19 hospital admissions per 100 beds have decreased 25% in the past week. But the Georgia admission rate remains 23% higher than the national rate. Among the hospital metrics that the WHCTF provides to us are COVID-19 demand for ventilators and ICU beds. You can see how Georgia compares to the US for these metrics below. You’ll notice that demand has held steady for the country since 20Dec, but demand has steadily increased for Georgia and remains high.
They further note that 14% of Georgia’s hospitals are reporting supply shortages, well below the national rate of 21%. So this is one area where Georgia is doing well. However, Georgia is not faring quite so well when it comes to hospital staff shortages - 31% compared to the national rate of 23%.
Today, there were 305 newly reported COVID-19 hospital admissions across the state and 37 admissions to the ICU. The number of patients currently hospitalized for COVID-19 decreased compared to yesterday, to 5428. This graph showing what looks like the peak so far for this surge is also showing a sharper decline compared to what we’ve seen in previous surges.
The graphic below shows us how the layout of the GEMA hospital regions for Georgia and the COVID-19 burden on hospitals. There are still four regions using an excess of their ICU beds. But Region J dropped out of the >90% group so now there are only 11 regions using >90% of their ICU beds. Many regions also saw a decline in the percentage of hospitalized patients who are being treated for COVID-19. But still, 13 of the 14 regions are classified in the darkest red category by the US Department of Health and Human Services color scheme. It’s wonderful to see trends dropping down, just understand that things remain intense for Georgia hospitals.
Deaths
The WHCTF notes that Georgia’s death rate more than doubled (+126%) over the past week. You can see how the weekly death rate has trended over time comparing Georgia to the United States in the graph below.
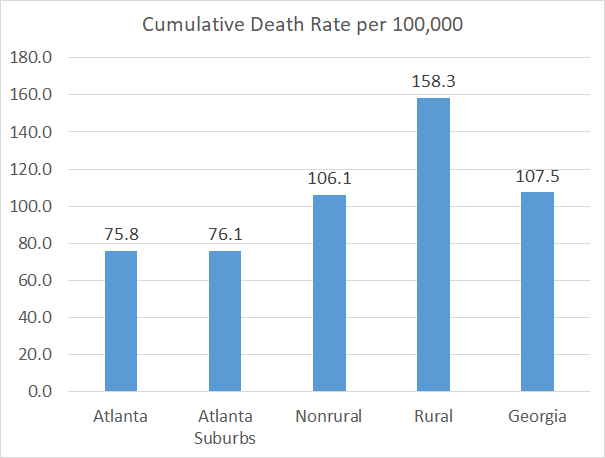
Today Georgia reported a net increase of 146 newly reported confirmed COVID-19 deaths. The updated statewide total is now 11,411. Thirty four percent of the deaths came from rural counties, 30% came from nonrural counties outside of the Atlanta metro, 25% came from Atlanta suburbs and 10% came from the Atlanta counties of Fulton and DeKalb.
As of today’s updated numbers from DPH, the average daily death rate per 100,000 over the past week in rural Georgia counties is so high that if it were its own country, it would have the fourth highest death rate in the world. The graph below shows us the disproportionate impact of COVID-19 deaths on rural communities since the start of the pandemic. The state average is the bar on the far right. The death rate in rural counties is more than twice as high as that of the Atlanta counties or suburbs.
References
https://publichealth.uga.edu/service-practice/outreach-programs/state-of-the-publics-health-conference/
https://opb.georgia.gov/document/governors-budget-reports/afy-2021-and-fy-2022-governors-budget-report/download
https://www.cdc.gov/hiv/statistics/overview/geographicdistribution.html
https://drive.google.com/file/d/1F60QjN4iGVzNlXzCkzQhhlApX25mhbQj/view?usp=sharing
https://beta.documentcloud.org/documents/20460344-georgia-1_17_21
https://covid.cdc.gov/covid-data-tracker/#vaccinations
https://dph.georgia.gov/covid-19-daily-status-report
https://covid-gagio.hub.arcgis.com/
Georgia COVID-19 Updates is a free newsletter that depends on reader support. If you wish to subscribe please click the link below. There are free and paid options available.
My Ph.D. is in Medical Microbiology and Immunology. I've worked at places like Creighton University, the Centers for Disease Control & Prevention and Mercer University School of Medicine. All thoughts are my professional opinion and should not be considered medical advice.