The Daily Digest, 16Dec2020
Georgia COVID-19 Updates
Vaccine Update
The Pfizer-BioNTech vaccine has already arrived across the country and is being administered to its first recipients. I have to say, seeing the photos and video of those healthcare workers and seniors being immunized made Monday the best day of 2020 on social media, at least for me. Usually, Halloween is my favorite day of the year, when I can see all the kids dressed up, see them growing up, etc. But no amount of pumpkin or fairy costumes can touch the joy and relief of what the first immunizations against this virus represent. This is when humanity strikes back. If you find yourself surprisingly emotional over this, you’re not alone. The Washington Post wrote this interesting article about the emotional release provided by this really, really important event.
Over the course of this pandemic, I have encouraged you to become more comfortable with data and to use data to make evidence-based decisions. The possible hesitancy surrounding taking the COVID-19 vaccines is worrying many in public health. But to me, I see some of this hesitancy as the people we’ve been teaching to be more data-driven doing exactly that. People want the data and they want to understand it. To that end, I’m linking the safety and efficacy data that Pfizer-BioNTech and Moderna briefed to the FDA in their applications for Emergency Use Authorization (EUA). Each document is >50 pages long and the data and verbiage will likely overwhelm most people. For those who are really overwhelmed, the area where I would focus most is the executive summary. But the document goes over their study design, the number of participants, and safety data including the types of reactions people experienced and how common they were.
For now, we’re going to go over the data that shows that the vaccine works (efficacy data), using figure 2 from both documents (see graphs below). These graphs show the number of people newly infected (aka incidence) with COVID-19 following injection with either the vaccine or the placebo (basically, salt water solution like what you would receive in a bag of IV fluids). The color coding isn’t consistent between the two graphs, they were submitted by different companies and likely didn’t coordinate. For the Pfizer-BioNTech graph, the placebo is the red line whereas the vaccine is the blue line. For the Moderna graph, the color coding is opposite - the blue line is the placebo and the red line is the vaccine. The x-axis shows the number of days after the first injection for each study participant. The y-axis shows the incidence rate over the duration of the study period, or how many of the people were infected with COVID-19 over time. You can learn more about how incidence rates are calculated by reading this lesson page from the CDC.
Looking at the top graph, the incidence of COVID-19 infection was the same between two groups until about day 10 at which time the vaccine group diverges in a big way from the placebo group. That makes sense based on what I talked about in my last vaccine update - it takes about 7-10 days to start producing antibodies after an exposure, including a vaccine. The Moderna graph is similar, but it’s harder to see that divergence around day 10 because the y-axis is more compressed. But they show the same thing. After about day 10, vaccine recipients begin to have some protection against the virus and after 100 days the protection provided is huge.
Vaccine efficacy measures how well the vaccine protects against infection, comparing those who received the vaccine versus placebo. The table below comes from the Pfizer-BioNTech document. Let’s orient ourselves. Time course is in the first column. The vaccine data (BNT162b2) are the second column. The placebo data are in the third column and vaccine efficacy is in the fourth column. Of over 21,000 people in each group, 50 people who received the vaccine and 275 people who received placebo later contracted COVID-19 (see row 1). Efficacy is calculated as the number of people infected in the placebo group minus those infected who received the vaccine, divided by the number of people infected in the placebo group. So, 275 - 50 / 275 = 82% (see fourth column). Mathematically, it’s sort of like saying how much did the vaccine reduce the number of people sick compared to if no vaccine was used at all. Now this 82% is over the entire course of the study. If we look at specific time intervals, you begin to see why two doses of the vaccine are needed. Of the 50 vaccinated people who contracted COVID-19 anyway, 39 of those got sick during the interval between dose 1 and dose 2, when vaccine efficacy was only 52.4%. Even within the 7 days after the second dose, vaccine efficacy shot up to 90.5%. Finally, once a person reached 7 days after the second vaccine dose, then the vaccine efficacy increased to 94.8%. So no matter what anyone tells you, the data show that you need two doses of the Pfizer-BioNTech and Moderna vaccines.
The Moderna document shows something else that is interesting, but perhaps not surprising, in Table 17. In this table, we’re looking at how well the vaccine conferred protection based on age group. Across all adults tested, the vaccine efficacy was 94.1%. For younger adults, <65, the vaccine efficacy was 95.6%. For adults 65 and older, the efficacy dropped to 86.4%. This is not so much a flaw of the vaccine as much as it is the impact of age on the immune system. As people get older, their immune system begins to decline and has a diminished capacity to respond to infection. But what this table tells us, for now, is the importance of achieving herd immunity - to protect the 4.4% of younger adults and 13.6% of older adults who for whatever reason did not mount an immune response to the vaccine or achieve protection from the virus. And until we know that herd immunity is achieved, it will still be critically important to continue to wear masks and socially distance ourselves. Because there will be no outward way to tell who the unlucky 4.4% or 13.6% are. It very well could be you.
In addition, we see that the vaccine protects against infection, but does it protect against transmission? Until we know more about that, even the vaccinated will need to continue to be cautious.
Data problems
Whew, your brain might need a time out after that vaccine update section. There are some problems with data feeds today for both Georgia and another state I follow, Kansas. For Georgia, the data feeds for the hospital capacity and patient census dashboards at the Georgia GIO hub are down. But none of the White House Coronavirus Task Force reports for this week have been made public yet - for any of the states. So I can’t talk about that today. I’m not sure how long the White House Coronavirus Task Force (WHCTF) is going to exist. With the presidential transition next month, it might be that the responsibilities of the Task Force are shifted back to the Centers for Disease Control and Prevention. Whether the reports continue or become daily/ weekly press briefings by CDC, I don’t know. I think the WHCTF reports have been an important historical record of the pandemic as it happened, serving as an equalizer for states with data dashboards of varying quality. Unfortunately, not every state has been willing to make those documents available for their citizens and the WHCTF hasn’t done so either.
Georgia
Today there were 23,433 newly reported PCR test results. Of those, 14.4% were positive. The state does not provide data on the number of antigen tests performed. However, we do know that they identified 37% of today’s net increase in cases…not a small number. Georgia’s percent positive rate has been trending upward since mid-October.
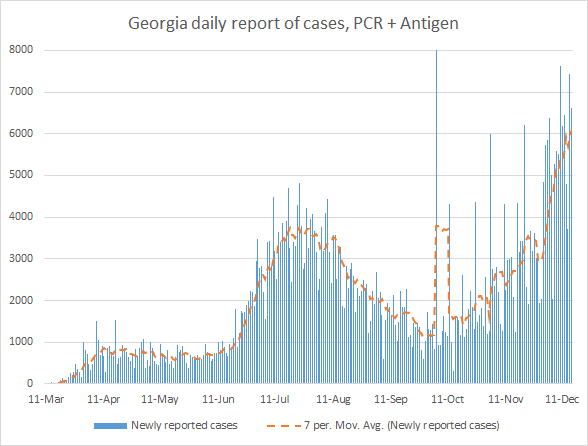
There was a net increase of 6624 newly reported cases compared to yesterday’s total, with 4186 identified by PCR and 2438 identified by antigen test. Thirty six percent of today’s cases came from nonrural counties. Atlanta suburbs and rural counties each contributed 25% of today’s cases, respectively. The graph below shows how our case curve has trended over time if PCR *and* antigen cases are included. The orange line is the 7-day moving average.
Cases are still increasing, but we have seen some slowing of the increase in the past few days. It’s too soon to know whether this is a leveling off, or a pause before further increases. In any case, our 7-day average as of today is 55% higher than the peak we experienced in the summer.
The broken Georgia data feeds are directly impacting our ability to see what’s happening with hospital and ventilator capacity as well as how many patients are in the hospital currently for COVID-19. Normally, you can see the dashboards for these data at the Georgia Geospatial Information Office data hub. But now you see a error message where the dashboards would normally be found:
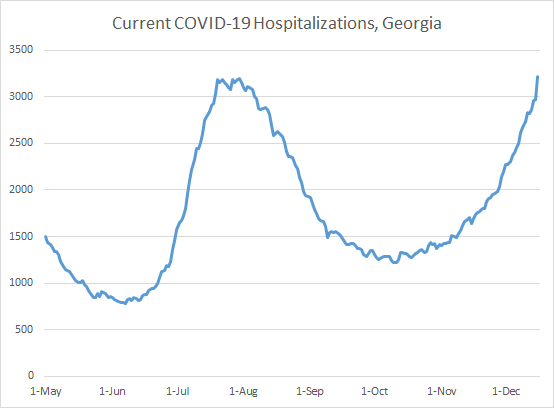
The “means to do so” could mean a lot of things. Hopefully this can be resolved quickly, because Georgia is in a dangerous place and the information we are missing is important. From my experience, working to perfect this data resource with the GIO office, this work was funded with CARES Act money. And that money ran out for this project this summer. So if we’re waiting for money, we might be here for a while. In the meantime, the Georgia Department of Public Health was able to issue this statement to members of the press indicating that today’s COVID-19 patient census is 3221, an increase of 8.5% over yesterday’s total. Many thanks to Mr. Bali for making that information public.


This is a new record for Georgia, the previous record of 3200 patients was set on 30Jul. So just as we are in uncharted territory for case rate now, we are also in uncharted territory for hospital demand due to COVID-19. You can see how the patient census number has trended over time below.
It’s an unfortunate day for the hospital dashboards to go down - we can’t see where the demand is most intense. During the summer surge, there were no governmental interventions to curb the spread of illness save for a handful of jurisdictions that instituted mask mandates. Instead, the thing that seemed to compel people to start adhering to public health guidance was the news reports of hospitals being overwhelmed. The Governor has indicated that he wants public action from ordinary Georgians to pull us out of this surge as it did in the summer - when we collectively limited disease transmission. But without this information on hospital demand and the burden of this disease, what will convince Georgians that this surge is serious enough to change their behavior? What will compel them to limit or cancel their holiday parties and gatherings? It’s a big ask, after all.
Beyond the currently hospitalized patient total, we had 307 new hospital admissions for COVID-19 and 40 new admissions to the ICU. These are both higher than usual numbers, but not record-setting. But they are driving the trendline upward for both metrics. The graph below shows how new admissions have varied over time.
I can’t provide any details on ICU bed capacity across the state, nor can I tell you how our usage of adult ventilators compares over time, due to the dashboard problems.
It was a mid-range day for newly reported confirmed deaths, at 52. The updated statewide total of confirmed deaths is 9302. The distribution across county types for these deaths mirrors the distribution for today’s newly reported cases: 36.7% from nonrural counties, 25% from Atlanta suburbs and 23% from rural counties.
I think that’s it for today. Please make good choices. We don’t know everything we want to know about hospital demand due to COVID-19, but the numbers we do have paint a very worrisome picture. We are likely in for at least a few more weeks of growing numbers, even if we change our behaviors today. However, it’s better to have 3 weeks of this rather than 6 or more.
References
Pfizer-BioNTech FDA EUA briefing document: https://www.fda.gov/media/144245/download
Moderna FDA EUA briefing document: https://www.fda.gov/media/144434/download
Washington Post article on the surprising emotions of the COVID-19 vaccine deployment: https://www.washingtonpost.com/lifestyle/style/covid-vaccine-video-reaction/2020/12/14/05754f66-3e59-11eb-9453-fc36ba051781_story.html
CDC Measures of Risk lesson: https://www.cdc.gov/csels/dsepd/ss1978/lesson3/section2.html#:~:text=Incidence%20refers%20to%20the%20occurrence,cases%20per%20unit%20of%20population.
DPH daily situation report: https://dph.georgia.gov/covid-19-daily-status-report
Georgia GIO COVID-19 data hub: https://covid-gagio.hub.arcgis.com/
Georgia COVID-19 Updates is a free newsletter that depends on reader support. If you wish to subscribe please click the link below. There are free and paid options available.
My Ph.D. is in Medical Microbiology and Immunology. I've worked at places like Creighton University, the Centers for Disease Control & Prevention and Mercer University School of Medicine. All thoughts are my professional opinion and should not be considered medical advice.