Vaccine Update
Today the Governor and Dr. Kathleen Toomey announced expanded vaccine eligibility beginning 15Mar2021 to include: all adults over the age of 55 and adults 16+ with underlying medical conditions associated with COVID-19 complications as defined by the CDC. Those conditions include asthma, cancer, cerebrovascular disease, COPD, cystic fibrosis, diabetes, hypertension, heart conditions, immunocompromised state, pregnancy, liver disease, neurologic conditions, overweight and obesity, pulmonary fibrosis, sickle cell disease, and thalassemia. Up until this point, everything has been done by the honor system. You should not have to provide documentation to prove your eligibility due to medical condition. You also do not need to have health insurance in order to get a vaccine. Then, “in early April” vaccine eligibility will expand to ALL people over the age of 16. Note: only the Pfizer vaccine is approved for 16-17 year olds. So if that is a priority make sure you’re looking for that particular vaccine. With expanded eligibility coming, if you are currently eligible please schedule your vaccine appointment ASAP.
I think this is a really positive development to see eligibility expanding. I know it doesn’t feel fast enough, but we just need to hang in there a bit longer.
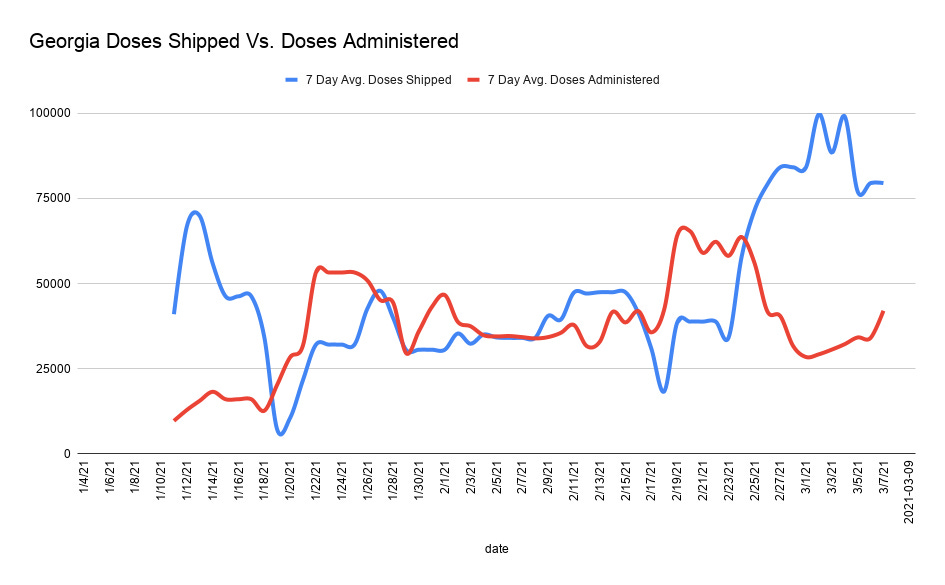
Leading up to today’s press conference, frustration has been growing over the glacial pace of Georgia’s vaccine rollout. The state is consistently at or near the bottom of the national rankings. According to CDC data (the complete data set) there are >1.3 million doses on hand that have been delivered to Georgia. According to DPH (a limited data set) there are 832,094 doses on hand that have yet to be administered. Either way, those numbers are absurd when each dose represents lives saved. Georgia is averaging between 40,000 - 50,000 doses administered per day, whereas the doses coming in daily far exceed that amount. The graph below was generated and provided by Grant Blankenship (Georgia Public Broadcasting, many thanks!) using CDC data curated by the Associated Press. From the graph, we can see that supply was definitely a problem over the past couple months. But that problem no longer exists since the last week of February.
There is no need to hang on to a surplus of 26 days’ worth of vaccine doses for second doses. The federal government is now able to give states a 3 weeks heads up of how many doses are coming. At most, the state needs to be hanging on to 5-6 days’ worth of doses.
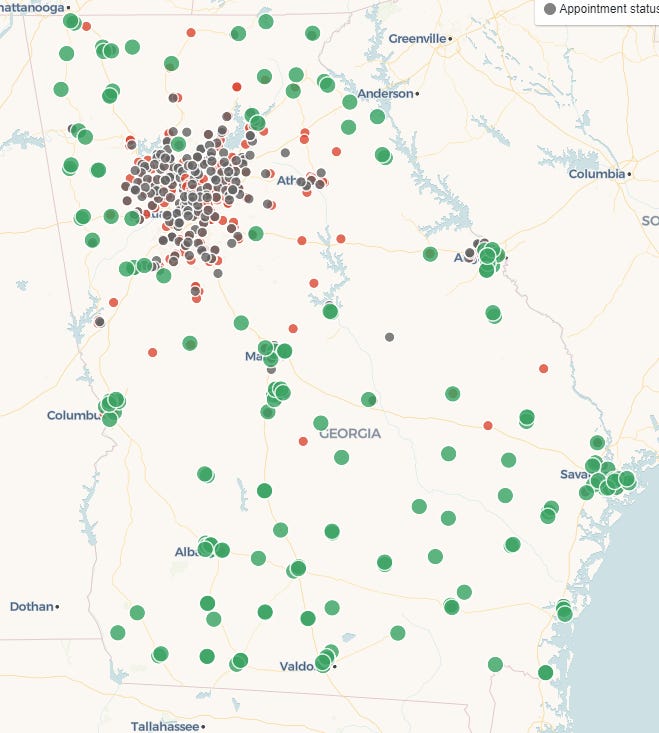
An additional problem seems to be that vaccines are not located where they need to be. The image below comes from a resource that allows you to search for vaccine appointments through retail pharmacies. You can use it to search for vaccines by zip code, throughout the US. In the map, green means appointments are available. Red means appointments are not available and gray means appointment status is unknown.
What we can see is that vaccine availability is plentiful in areas outside of the Atlanta metro. But even some rural areas are seeing shortages. But there is a serious shortage of vaccine appointments in the Atlanta metro. If you have the means to travel outside of the metro for one of these appointments or can help someone else to do so, I hope that you will. But this presents yet another barrier to access for far too many people. As I’ve suspected for a while, the problem seems to be inefficiency and not matching supply to demand. But there may be several factors playing into the disparities here, especially for green areas: (1) vaccine hesitancy or lack of demand among eligible population, (2) the area has vaccinated the majority of those who are eligible and willing, (3) there are too many barriers to access for the eligible population.
White House State Report
The White House state reports are out today. They are changing the timeline somewhat to finalize reports on Fridays. But we still only just got the vaccine today on the following Wednesday. Perhaps we will see reports earlier in the week in the future.
Top 5 states for new case rate: New Jersey, New York, Rhode Island, Delaware, Georgia. There are 33 states in the red zone.
Top 5 states for test positivity: Texas, Alabama, Florida, Oklahoma, New Jersey. Georgia is ranked #8. There are no states in the red zone!!
Top 5 states for COVID-19 hospital admissions: DC, Maryland, Virginia, Pennsylvania, and Puerto Rico. Georgia is ranked #9. There are 3 states in the red zone.
Top 5 states for new death rate: Virginia, Oklahoma, Texas, Alabama, California. Georgia is ranked #6. There are 30 states + DC in the red zone.
Top states for percent of population who have received 1+ vaccine: Alaska, New Mexico, Connecticut, South Dakota. The bottom 5 include Puerto Rico, Georgia, DC, Texas and Utah.
Testing
The map below shows test positivity by county. Ideally, you want to be in the green or gray zones. Anything above that is above the 5% goal line. The map is much improved compared to a month ago. The graphs on the right show us how test positivity and test output have varied over time for Georgia compared to the US.
The test positivity rate is continuing to decline for both the state and the US. The US has already dipped below the 5% goal line and Georgia most likely will do so in the next week’s report. As for test output, the gap between the national and state test output is widening. So far, Georgia isn’t seeing test positivity increase due to reduced testing as might be predicted.
Today Georgia reported 17,503 newly reported PCR test results, 5.5% of which were positive. There were 11,847 newly reported antigen test results, 5.5% of which were positive. This is the second day in a row that the percent positivity between these two numbers has been identical and that is odd for data that virtually never agree.
Cases
The map on the left comes from the White House state report showing new case rate. Some of the reddest parts of the state surround the Atlanta metro or are clustered near the southern border with Florida. The graphs on the right show you where Georgia has been over time compared to the US for new case rate (top) and infections at skilled nursing facilities (SNFs).
Case rate is declining but leveling off for both the US and the state. But whereas the nation is leveling off at a level that is 76% above its pre-surge baseline, Georgia is leveling off at a rate that is 149% above the pre-surge baseline. Since this report was generated though, cases have continued to decrease for Georgia. So perhaps the next week’s White House report will reflect that. The percentage of SNFs with at least one case of COVID-19 has plummeted too, due to both the vaccine and reduced community transmission. But the decrease stopped this week, at about the same level as the pre-surge baseline. Hopefully it’s just a temporary pause.
Today Georgia reported a net increase of 1157 newly reported PCR cases and 583 newly reported antigen cases for a combined total of 1740. The 7-day case rate is now just 62% above the pre-surge baseline. Remember, the graph below and its numbers use daily updates from DPH. The White House reports use weekly totals, closing out last Friday. So the difference in how high above the pre-surge baseline we are, is most likely due to the timing of data collection. In any case, we want to see this number continue to drop. Much of the worry over the past month has been what was going to happen with the dominance of the B.1.1.7 variant of the virus (the variant that originated in the UK). It is expected to be the dominant virus in Georgia this month. So seeing the case rate decline is encouraging. But I still don’t think we’re out of the woods on the B.1.1.7 variant’s potential impact until early to mid-April. Hopefully the expanded vaccine eligibility will help to make the winter surge our last surge.
Case rate is lowest in rural counties and highest in the Atlanta suburbs.
Hospitalizations
Only about half of Georgia’s hospitals reported data last week. So you’ll notice a lot of blank space on the map below for COVID-19 admission rate to hospitals. As such, it’s kind of hard to know how much of this week’s decrease (see graph on the right) is real. I hope that it is, of course.
There were 123 newly reported hospital admissions for COVID-19 today and 16 admissions to the ICU. These are both low numbers which is fantastic. Things continue to trend down for most hospital regions (data not shown).
Deaths
The map below shows you the new death rate by county last week. Anything in the red zone is considered high. The graphs on the right show how Georgia has compared to the US over time for confirmed death rate and the proportion of SNFs that have at least one COVID-19 death each week.
The death rate continues its descent for both the US and the state of Georgia. Neither are close to their pre-surge baseline, but deaths tend to take longer to come down than cases. As we saw for cases in SNFs, the descent in deaths leveled off this week in Georgia.
Today Georgia reported a net increase of 59 newly reported confirmed COVID-19 deaths and there was a data correction in the probable column to subtract one death (net change compared to yesterday). This death total is a typical number compared to what we’ve been seeing lately. But our current “typical” is much lower than where it has been in recent weeks. The 7-day death rate continues to trend downward and now the state is at a level that is 50% above the pre-surge baseline. We are getting closer every day. As we have seen for previous surges, the death rate tends to be higher in rural counties compared to other county types in the state.
Tomorrow marks the one-year mark of when I started tracking data for the pandemic. In the early days, Georgia DPH was posting numbers each day but there was no context of how things were trending over time. I hadn’t met or talked to anyone at the agency by that time but having worked outbreaks before, I knew they were probably overwhelmed. I was happy to help out where I could, explaining trends to those in my network and passing on any and all guidance that was coming from DPH and CDC.
It was around this time last year that I sat in a conference room of 8 medical students (my student group) who were scared and looking to me to provide reassurance but also to level with them about what I saw and what could happen. “It’s not real until Dr. Schmidtke says it’s real,” I remember one of them saying. It was around this time that my faculty mentor (a critical care specialist) played this off as something that wasn’t probably going to be all that serious. And then I explained how R0 worked and what the data from China were telling us about expected mortality and hospital demand. He left my office with a change of heart. It was a year ago yesterday that I ate my last meal in a restaurant (Natalia’s in Macon) where a colleague and I were interviewing a faculty candidate. On Friday, March 13th, a colleague and I delivered a seminar on the virology and public health aspects of COVID-19 to the entire student body, faculty and staff at Mercer University. I opened by telling people that I couldn’t promise them that the things I had to say would make them feel better, but I would tell it to them straight. They would have the best information science had to offer at that point. At one point, when talking about who we were most worried about, I looked at my students and said, “it’s not about you, it’s about people like my dad” and then trailed off as emotion made my voice quaver. That was the moment that the pandemic moved from the academic interest to my reality. I looked out and saw colleagues and coworkers who I cared about deeply who were older, had chronic health conditions, etc. I felt extraordinary pressure (that I heaped onto myself) to protect as many of these precious and loved people as I could with information and data so that they could make informed choices about their risks and how to avoid infection and avoid transmitting it to others. Remember, at this time, we didn’t know how bad it was going to be. But the images coming out of Italy were scary. Two days after our seminar, the decision was made to close the campus and I breathed enormous relief.
I bring up these memories because what I remember about life a year ago was the chaos, uncertainty, anxiety and the thirst for someone to tell us all that we would be okay. I remember scenes in hospitals and commercials that brought tears to my eyes. I remember a sense that we were all in this together and that I would do what I could to keep my people safe. To me, data provide comfort. A situation may be bad. But if I can see the trends, then I have a better sense of what to expect. We are not done yet with this pandemic, but I’m relieved to see case and death rates decreasing again, hopefully for the final time. As we vaccinate more and more people, I can’t tell you what it means to be able to tell you that things are going to be okay. In the meantime, continue to make decisions that will protect you and your community. We are getting closer to the end of this pandemic, but we need to hold on just a bit longer.
References
https://dph.georgia.gov/covid-19-daily-status-report
https://covid-gagio.hub.arcgis.com/
https://beta.healthdata.gov/Community/COVID-19-State-Profile-Report-Georgia/xhcs-tqqe
https://covid.cdc.gov/covid-data-tracker/#vaccinations
Georgia COVID-19 Updates is a free newsletter that depends on reader support. If you wish to subscribe please click the link below. There are free and paid options available.
My Ph.D. is in Medical Microbiology and Immunology. I've worked at places like Creighton University, the Centers for Disease Control & Prevention and Mercer University School of Medicine. All thoughts are my professional opinion and should not be considered medical advice.