Hello and Happy New Year! I’m sure many of us are happy to close the door on 2020 and eager for better things in 2021. I just wanted to take a moment to thank you for reading the newsletter, whether you’ve been here since the beginning or only recently. In 2020, my “student body” grew from the 60 medical students I was responsible for at Mercer University School of Medicine to >60,000.
At one point, I remember having a conversation with my medical students about the difference between the way that a medical doctor sees the world and the way that a public health professional sees the world. That’s not to say there aren’t lots of MDs in public health (and veterinarians and nurses too!). And we are very much on the same team, but addressing different parts of the problem. But whereas a medical doctor in the traditional sense is focused on the patient in front of them, for people in public health (or those who wear both hats) their “patient” is an entire community. The way we gather data and the way that we diagnose problems is different too. What both have in common, however, is that they rely on a team approach when caring for their patient. In the medical setting, that’s the physician, nurses, phlebotomists, laboratory staff, food service, supply management, orderlies and administrators. In the public health setting, it’s epidemiologists, data scientists and statisticians, contact tracers, IT staff, laboratory staff, communications staff, inspectors, analysts, public policy experts, etc. I’m probably leaving out members of each team who are tremendously important - please forgive any omissions here.
When public health works well, you often don’t ever realize that we did anything. If public health isn’t in the news, then we’ve done a good job. It’s hard to count the number of lives saved by a vaccination or the quality of life improvements due to early detection of genetic disorders through the Newborn Screening Program, or countless other public health programs. But that silent success for public health is part of what led to the failures of the American response to the COVID-19 pandemic. When politicians brag about their achievements to their constituents, investments in public health are not among the glamorous highlights. But we still need to demand them. And it can be hard for public health to advocate for itself when so many of us work for government organizations (local, state, or federal) where political advocacy is frowned upon. So, instead, we’ve seen big cuts to staffing and funding for public health over the past decade and that has meant that everything about our pandemic response has been painfully slow and ill-equipped, from testing to PPE stockpiles and procurement, to dashboard design to vaccine deployment. Infrastructure is not built overnight and neither is expertise. I don’t say any of this to offer excuses. But I wish so much that America (and Georgia) could have a do-over on this pandemic with the proper funding and staffing in place. I can’t help but wonder how different things would be if public health was able to operate with full support and optimal efficiency. I wish that the leaders in public health had been able to communicate directly with the public on a regular basis and that there had been unified messaging to limit the impact of disinformation and politicization. Instead, the responsibility of communicating the pandemic to the public has fallen to people like me and so many others in other states. This has been a team effort too, but not as coordinated as a federal response would have been. Experts from all sorts of disciplines have lent their expertise to this public effort because the stakes are so high and it is totally worth the risks of becoming a public figure even if it saves just one life in this pandemic. This uncoordinated science communication network is beautiful in its own way. But it is not the way things are meant to be done and it has cost lives to not have consistent and unified messaging that reached every state and every county in this country. I will always wish that I could have done more, covered more states, had better access to data, etc.
In a crisis, so many people want to do whatever they can to help, to pitch in. I can’t save a COVID-19 patient who is struggling to breathe. That’s not where I specialized in my education. But my medical students and nursing students will. If you are one of my former students - I am so very proud of you and the ways you are impacting or will impact your communities. I think of you every day since this pandemic began and hope that you are safe. Instead, the way I’ve been able to pitch in is to communicate the risks, teach you how to read and interpret data for yourself, and encourage you to make evidence-based decisions. So as much as my readers may think that they have gained from my work, I assure you that working to ensure that you are safe (or at least know your risks) has been some of the most important work that I have ever done. It has been the way that I have pitched in during this period in history. So thank you for this opportunity to serve my community and to make a difference.
Enough of this sappy talk. Let’s get to the data.
Testing
It was a big day for testing, with 51,664 new PCR test results reported through Electronic Laboratory Reporting (ELR). Of today’s PCR tests, 17.7% were positive. Our percent positive rate is trending higher than we saw during the height of the summer surge. And we are a long way off from the 5% goal right now.
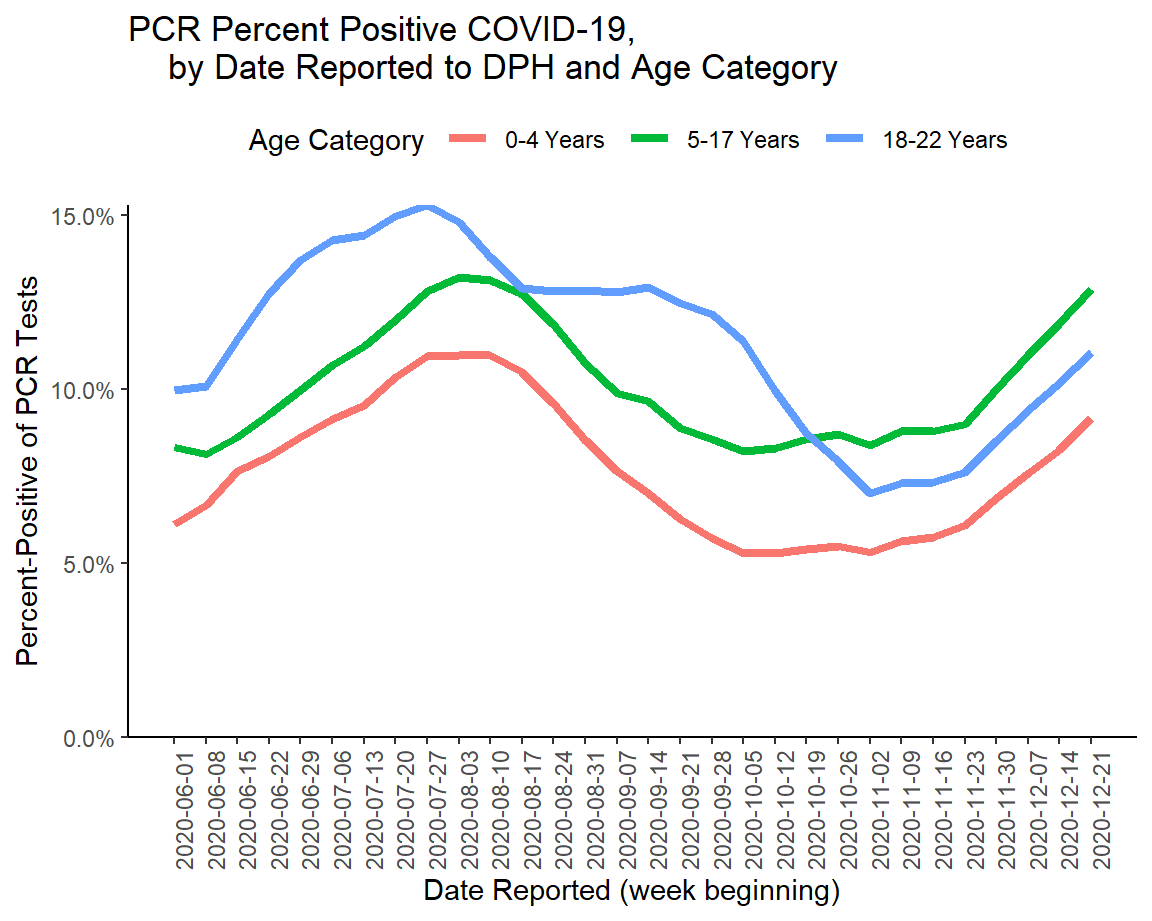
We also see that the percent positive rate is increasing among children in this week’s school-aged data surveillance report. It is highest among K-12 aged children in the graph below.
The good news is that we have brought our percent positive rate down before and we can do it again. But as we see from the graph below, it is not quick or easy work to reverse a surge. There is no indication that there will be any sort of government intervention to put the brakes on this surge we’re in now. Instead, we get there by limiting disease transmission in our communities through the collective actions of individuals. Every step you take to reduce transmission gets us closer.
The Georgia DPH does not provide information on the number of antigen tests performed nor how many were positive. But we do know that this test identified 22% of today’s newly reported cases, for one in five.
Cases
It was nearly a record setting day for cases, with a net increase of 8719 PCR cases and 2418 antigen cases for a combined total of 11,137 newly reported cases. The record was set yesterday, at 11,709. Among today’s newly reported cases, 33% came from nonrural counties outside of the Atlanta metro, 29% came from the Atlanta suburbs, and 22% came from rural counties.
As of today’s update, our statewide 7-day case rate per 100,000 is now more than twice as high as the height of the summer surge (+114%).
The Georgia Department of Public Health only uses PCR cases when doing all of their graphs and maps on their daily status report. The exclusion of the antigen cases, which they investigate the same way as PCR cases, gives a misleading undercount of the disease severity in the state. The map below includes both PCR and antigen cases to calculate the 14 day case rate per 100,000. The color break points are set up the same way as the DPH map. You can click on the map to reroute to the live image where you can click/hover over your county of interest to see its number.
What we see is that 77 counties are in the highest color tier, with a 14 day case rate per 100,000 that is >930. These dark purple counties are distributed throughout the state but less so in southwestern Georgia and along the coast. There are also a lot of rural counties in the top tier.
Using PCR + antigen case data from the school aged COVID-19 data surveillance report, we see that case rate has been surging since early November for all age groups. We also see that the case rate increase has been nearly identical between 18-22 year olds and older adults but less of an increase has been observed among 0-17 year olds.
The most recent report shows a leveling of the case rate increase. However, it is too soon to tell if that is part of a trend or if we will see the numbers bounce back up in the next report. And that latter situation is likely, given the record setting cases reported this week.
Hospitalizations
Today there were 278 new COVID-19 hospital admissions and 31 new admissions to the ICU. The number of patients currently hospitalized for COVID-19 is 4563, a small decrease from yesterday’s number. COVID-19 patients make up 28% of all patients who are hospitalized today. The US Department of Health and Human Services defines anything over 16% to be in the red zone and all of Georgia’s hospital regions, as well as the state average, are in the red zone. The regions with the highest COVID-19 patient census are regions M (41%), E (39%), and H (39%). Region J (coastal Georgia) is currently not in the dark red zone, but has been steadily inching up and will likely join the rest of the state if current trends continue.
In fact, only hospital regions I, J and K have avoided surpassing their summer peak for patient census. The other 11 hospital regions are all treating more COVID-19 patients than they have ever had.
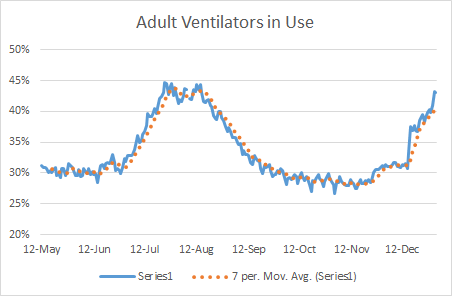
There are 8 (of 14) hospital regions using >90% of their ICU beds and three are using 100% or more (A, G, and H). Statewide, about 89% of the ICU beds are full. Forty two percent of the state’s adult ventilators are in use today. We have not yet surpassed the summer surge peak for ventilator use, but if trends continue we will probably surpass that number (45%) next week. According to the 30Dec2020 HHS Community Profile report, COVID-19 patients are using 39% of the state’s ICU beds and 13% of the state’s ventilators.
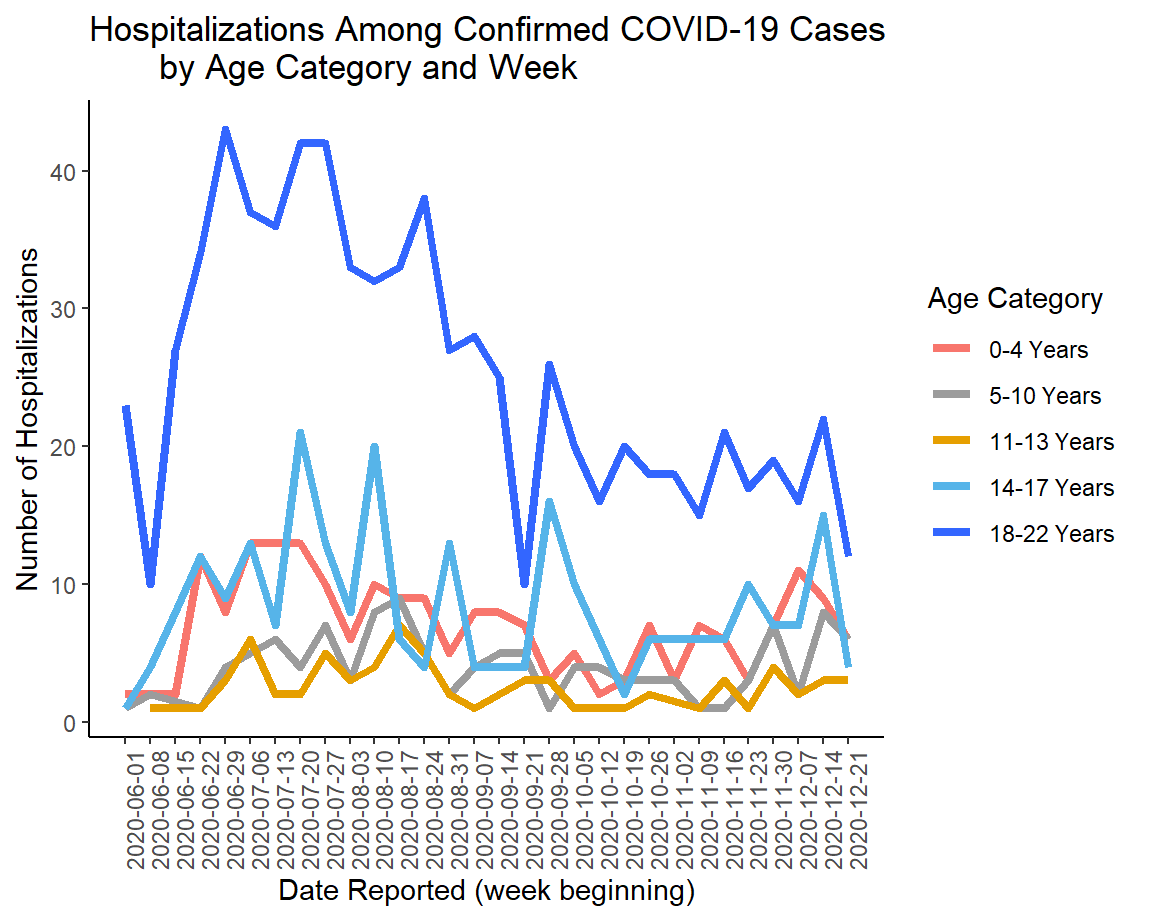
There are some interesting and compelling trends for children when it comes to COVID-19 and the need for a hospital in the school aged data surveillance report. The graph below shows the percentage of all Emergency Room visits among children and 18-22 year olds that are for COVID-19.
We can see that the percent of ER visits for COVID-19 is rising dramatically for all age groups and all of them have surpassed their peak during the summer surge. There is a decrease in the most recent week for 5-10 and 11-13 year olds (approximately elementary and middle school aged, respectively). But the percentage has more than doubled for 14-17 year olds in the past month and doubled for those 18-22.
Whereas the number of kids needing an ER for their COVID-19 illness is trending up dramatically, the same trend is not observed for hospital admissions. It’s possible this is due to their cases being serious enough to warrant an ER visit, but stable enough to be sent home.
Deaths
It was a comparatively small day for deaths today, with 17 newly reported confirmed deaths. Given that it’s a holiday, this is likely similar to the weekend effect that we see when nursing homes and other facilities have delays in reporting. Of today’s newly reported confirmed deaths, 41% came from rural counties and 29% came from the Atlanta suburbs.
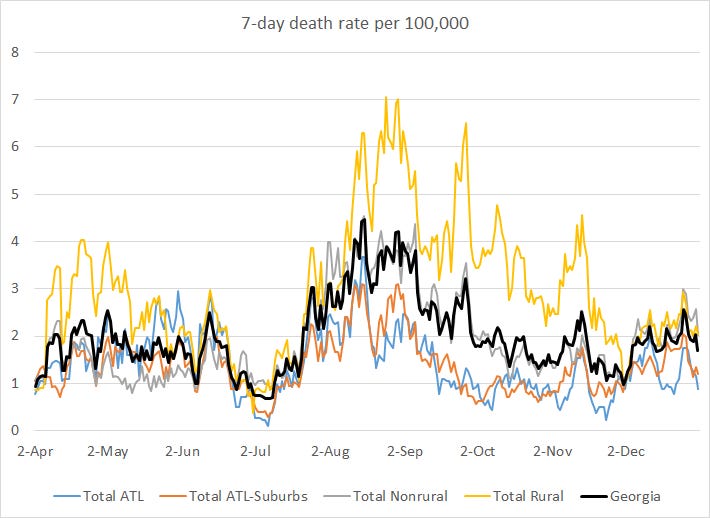
When the summer surge happened, we saw a dramatic rise in death rate about three weeks after the surge in cases began. We are seeing an increase in the death rate this time, but it’s not nearly as dramatic this time which is weird since this case surge is so much bigger. It’s possible this might take off in the weeks to come, given what has happened in states nearby and especially as hospitals become overwhelmed. But, for now, it seems things aren’t as bad as we had before. I’m not sure if that’s good news to celebrate yet or just the calm before the storm. Just remember that survival and death are not the only outcomes of a COVID-19 infection. There are many, many people who have lasting health problems after their infection is gone.
Yesterday there was a press conference from the Governor and Public Health Commissioner, Dr. Kathleen Toomey, where they indicated that there is lots of demand for the vaccine among healthcare workers in metro Atlanta but it was sitting in freezers in rural counties due to vaccine hesitancy by healthcare workers in those communities. If you find that you have concerns and questions about the vaccine, I want to direct you to this newsletter where I discuss who and what ACIP is, the vaccine efficacy data, how the vaccine works inside of your body, and how the prioritization decisions were made. If there are additional questions, please don’t hesitate to email me so I can help find the information you need to feel safe and confident.
Regardless, it is very exciting to see the demand for the vaccine in metro Atlanta. A vaccine is worthless until we convert it into a vaccination (meaning, it’s in someone’s arm). For this reason, the state is moving on to include first responders and people >65 in the next couple weeks. Hopefully we have more details in the coming days. The more people we can vaccinate and get to herd immunity safely, the safer our workplaces will be and the faster our economy can recover. I worry that rural counties will be left behind and continue to suffer the ugly consequences of the pandemic, if vaccine hesitancy continues there. Hopefully, more is being done behind the scenes to develop better science communication to rural counties to build confidence and trust in the vaccines. Because the death rate in rural Georgia counties is more than twice as high as the Atlanta metro. There are definitely lives to save in these communities, if they are willing to limit transmission and take the vaccine.
References
https://dph.georgia.gov/covid-19-daily-status-report
https://covid-gagio.hub.arcgis.com/
https://epidemiologyschoolreport.s3.amazonaws.com/SchoolAgeSurveillance1221.html#statewide-data
https://datawrapper.dwcdn.net/hkfx2/1/
https://kansascovid19updates.substack.com/p/all-about-covid-19-vaccines
https://www.wsbtv.com/news/local/covid-19-vaccines-not-being-used-sitting-freezers-some-areas-georgia/44GWKHOBKRB4HLRA7R6ZMKH5PY/
Georgia COVID-19 Updates is a free newsletter that depends on reader support. If you wish to subscribe please click the link below. There are free and paid options available.
My Ph.D. is in Medical Microbiology and Immunology. I've worked at places like Creighton University, the Centers for Disease Control & Prevention and Mercer University School of Medicine. All thoughts are my professional opinion and should not be considered medical advice.