Nationally, things are continuing to get better. First, let’s look at community transmission level. Remember, this map and color coding is based on recent case rate and recent test positivity, to estimate the risk of exposure to the virus in each county. You can see from the graph and the map that the vast majority is still in the red or orange category. This means that there is still a lot of disease being passed around across the country.
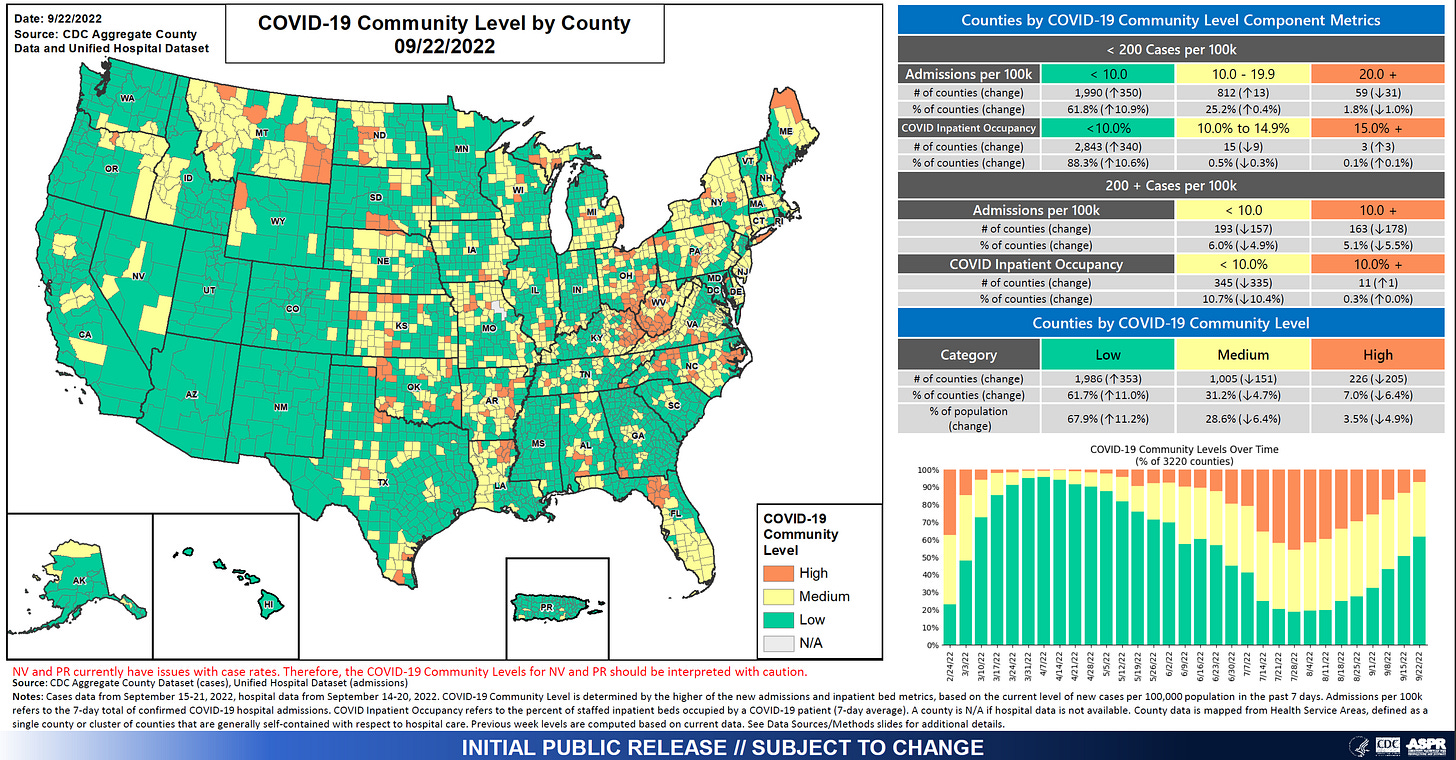
The second way to look at the national picture is to look at CDC’s Community Levels map, which estimates the difficulty one would have in finding a hospital bed (for any reason) if they needed one. It uses a combination of COVID-19 admission rates, percent of patients hospitalized for COVID-19 and recent case rate. In this color scale, green is good or low risk of difficulty. In the graph to the right, we can see that the proportion of counties that are green is growing steadily since early August.
One thing to note is that the community levels graph is improving much faster than the community transmission graph. They are measuring different things. But one could interpret this to mean that while a lot of people are still getting sick, fewer of them are needing a hospital bed. This could be due to a combination of vaccine-provided immunity and naturally acquired immunity (i.e. people who have recovered from infection).
We are also seeing a sustained lull when it comes to death rate per 100,000 across all regions of the country. Compared to where we have been, death rates are relatively low. Though, I think one could argue that any deaths from a preventable disease are unacceptable. Whereas we did see a bit of a case bump over the summer, we did not see a corresponding death bump.
All the same, over the most recent 7 days for which the CDC is providing data (9/16 - 9/22), the US has recorded 2496 deaths. As a point of reference, the death toll from September 11, 2001 was 2977. So we’re not that far off from a 9/11 scale of death each week. To date, 1,050,631 Americans have died from COVID-19.
Given that the US is continuing to lose so many people to COVID-19, it was surprising (and yet not surprising) to hear President Biden tell Americans that “The pandemic is over. We still have a problem with COVID. We’re still doing a lot of work on it. But the pandemic is over.” It was surprising because his claim isn’t supported by data and because he doesn’t have the power to declare that a pandemic is over, and certainly not when COVID-19 continues to cause problems throughout the world, including in many countries who have yet to receive a single vaccine dose. It was unsurprising because President Biden’s posturing regarding the pandemic has always been based on what was politically expedient. In short, if you want people to stop talking about the pandemic and recognizing that the government has fallen short on its responsibility, you tell people the pandemic is over. Is this really all that different from the previous president who also minimized the importance of the pandemic for similar reasons?
Of course, an easily predictable consequence of a statement like this is that when you tell people that the pandemic is over and you’re the President of the United States, they have a tendency to believe you whether you’re correct or not. That includes other politicians who would rather not fund emergency spending for COVID-19 mitigation efforts. The Biden Administration cannot simultaneously tell people the pandemic is over and still ask for $22B+ in funding for the COVID-19 response and expect to get a good result.
It also won’t help efforts to get Americans to take the updated bivalent COVID-19 vaccine booster.
The updated bivalent COVID-19 booster was authorized for use earlier this month. So far, people are getting them, but likely not enough. The graph below comes from the CDC and it shows the number of doses administered each day with a 7-day moving average shown in the red line.
So far, 4.4M Americans have received an updated booster dose. That’s roughly 1.3% of the US population. It is 2.2% of the population who received the primary vaccine series. But it is 4% of those who received a previous booster dose. So those who have been diligent about staying up to date on their COVID-19 shots are more likely to do so. We may see some improvement in these numbers with time. Many might wait until closer to flu season to get both their flu shot and their COVID-19 booster at the same time. It remains to be seen what impact President Biden’s comments will have on the booster roll out effort.
As for me and my family, we went a couple weeks ago to get our flu and COVID-19 bivalent boosters done. We have an 11 year old who is too young yet to get the updated booster. But he will get it as soon as he is authorized. For those who might ask - I did get mine in the same arm. My husband and older son did one in each arm.
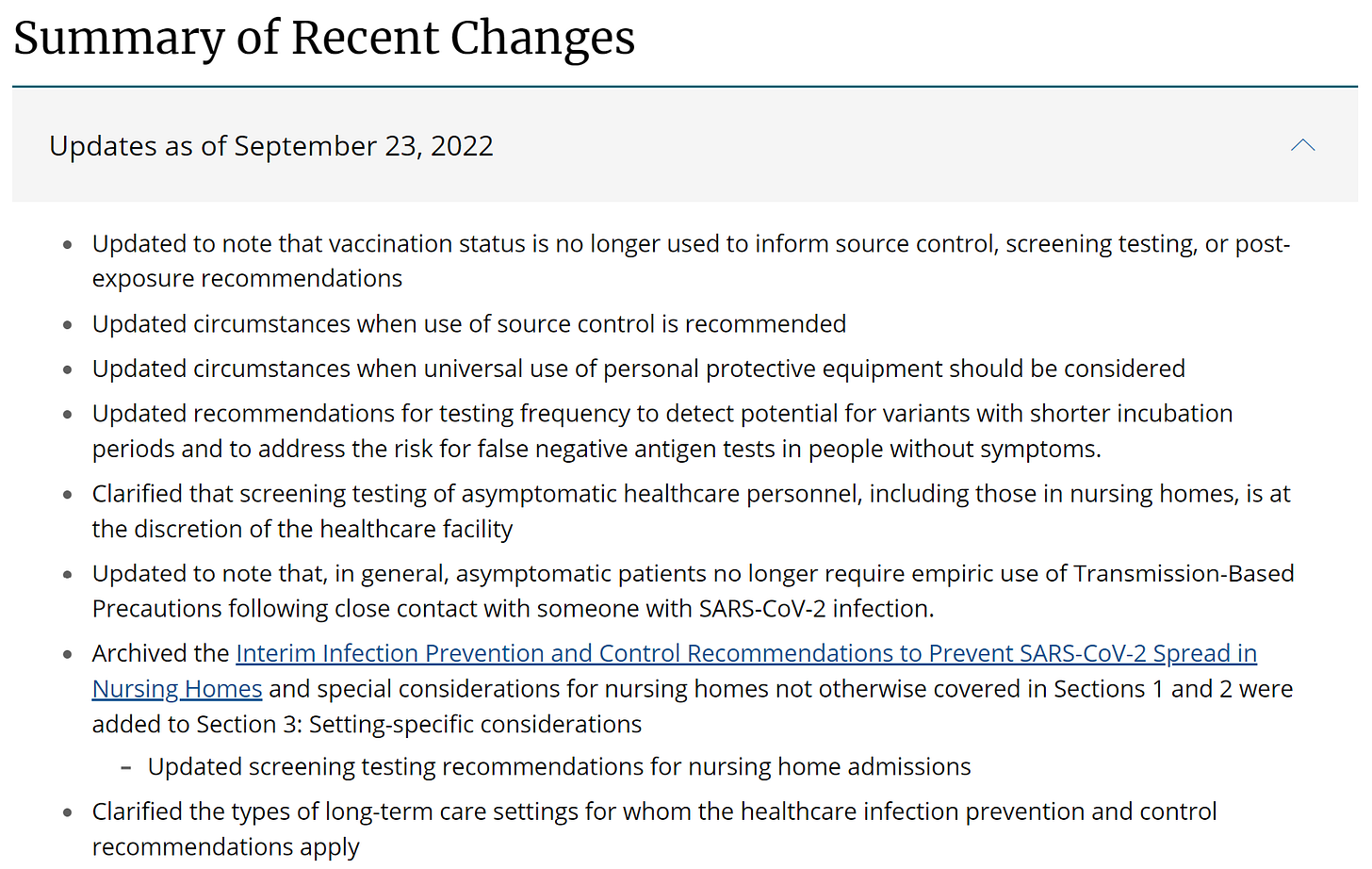
The Biden Administration’s “You Do You” approach to COVID-19 response is also demonstrated in the latest CDC updates to healthcare facility guidance. This week they released a host of changes. Among the more controversial changes is that hospitals can end universal masking, particularly when community transmission levels (red-orange-yellow-blue map above) are low. Note that, at present, that represents 9% of US counties (translation: keep your mask on for now).
There are at least two really glaring problems with this. First, we are depending on a metric that is based on recent case data, when we know that testing volume is not high enough to identify most disease. COVID-19 testing centers have closed. It is a recommendation to follow a data point that the CDC knows is imperfect and the Biden Administration has worked to ensure will be inaccurate. You can’t find disease if you aren’t looking for it. The second problem is what is happening to the immunocompromised. Society has gradually forced them out of population centers by creating unsafe spaces that are teeming with disease. As masks have come off, people knowingly travel while sick, and people ignore testing because they would rather not know (and isolate) the world is a scary and dangerous place for the immunocompromised. Society’s messages have been for these folks to wear a mask if they want to or just stay home. Ugly though these things may be, we have some modern conveniences that may have made this work for those whose risk was too high to go into some of these places including grocery ordering, outdoor dining and concerts, etc. But the immunocompromised are some of the most medically vulnerable folks we have. They don’t have another option when it comes to accessing healthcare. They need hospitals and clinics to treat their conditions while not exposing them to an infection that could kill them. I had honestly expected that universal masking was just going to become the norm in hospitals and nursing homes.
The past two years of masking had big impacts on influenza, drastically dropping the number of annual infections and deaths. However, now that masks are present in lesser numbers we should expect many respiratory infections to come roaring back, including influenza. The CDC tracks influenza data at their FluView website.
District of Columbia is already seeing very high levels of influenza like illness. Texas, Hawaii and Georgia are in the moderate category. Early in the pandemic, many of us in public health were worried about a so-called Twindemic, where we saw the combined impacts of COVID-19 and influenza. That didn’t materialize in the first year, partly because of masking but also due to heightened awareness of COVID-19 symptoms that shared similarity with influenza and people staying home when they were sick. We also still had virtual learning in some schools. Not saying virtual learning is good or bad, but it did contribute to decreasing disease. None of those things are in place this year. So there is some concern that this year will be the year we see the Twindemic.
I do think that getting the flu shot and the COVID-19 booster are going to help us to decrease the number of infections and deaths this winter. But if few people are taking them, we have to consider a vaccine plus strategy where we layer additional strategies on top of vaccines. I think this pandemic has shown us that we do have very effective tools to limit disease transmission. But we lack the community willpower to use them in a way that protects the most vulnerable. In this sense, we are on our own. And when that’s the case it is the people who are well-resourced who suffer the least impact. They are the ones who have health insurance, paid time off, and don’t live paycheck to paycheck. The government’s current indifference to the medically and economically vulnerable will further exacerbate the disparities in health that we see for people of color, rural populations, and the poor.
Unless otherwise stated, all data presented are publicly available from the Georgia Department of Public Health and the Georgia Geospatial Information Office. Graphs and images that were not produced by me are linked to the original source if you click on them. Thank you for your support of the COVID Digest.
My Ph.D. is in Medical Microbiology and Immunology and I am Chair of the Division of Natural Sciences and Mathematics at the University of Saint Mary. I've worked at places like Creighton University, the Centers for Disease Control & Prevention and Mercer University School of Medicine. All thoughts are my professional opinion, do not represent the views or opinions of my employer and should not be considered medical advice.









One thing I am noticing, we are approaching year 3 of the pandemic and my husband-an internal medicine doctor in a deep red part of Georgia-was able to stay well as he treated patients throughout the first two years but this year the toll of this has begun to really tell on him as so many of the people he sees are so much sicker and more complicated to treat post Covid. Pre pandemic we had flu season every winter but the summers usually eased off somewhat so you could catch your breath and recharge a bit. I feel like there are other physicians and care givers of all sorts who are experiencing the same sense of burnout. Offices here in Whitfield and Murray counties are still masking for now but physician's offices in Floyd and Gordon recommend you mask but then very few of even their own staff mask. We discuss regularly how to navigate through all this to ensure he has retirement years to look forward to. Your deep sense of frustration is shared.
Thank you for powerfully speaking truth to power