COVID in the US
Let’s begin by looking at the national map for COVID-19 Community Transmission Levels. This map estimates the likelihood that you will be EXPOSED to COVID-19. Prior to February 2022, any county in the orange or red would be advised to have a mask requirement in place. At present, that represents 97% of US counties. Even using the CDC’s made up metric, Community Levels (likelihood you’ll have difficulty accessing a hospital bed), 42% of US counties should be wearing masks. And yet…not many people are wearing masks.
According to the New York Times COVID tracker, the US has been exceeding 100,000 new cases each day since 25Jun. Keep in mind, this is likely a vast undercount. The 7-day average for new hospitalizations for COVID-19 is more than 40,000 per day and rising fast. “Endemic” means expected low levels of disease. This is unexpected high levels of disease. We are not endemic right now. This is an epidemic. We should be doing something.
Georgia
In Georgia, there’s a lot of disease throughout the state. But it seems to be especially bad in southwest and middle Georgia.
In fact, if we look at the change in 7-day case rate per 100,000 residents over the past 2 weeks, we can see that case rate is rising everywhere, but most significantly in hospital region K (the southwest corner of the state). This region was hit particularly hard in the initial wave of the pandemic.
We can also see that multiple parts of the state are seeing a large multiweek rise in their COVID-19 patient census. This means the percent of patients in the hospital who are there because of COVID-19. Let me tell you, every surge Georgia has had started out this way, slowly edging out of dark green into light green, multiple regions in yellow and then eventually most if not all of the state is in the red zone.
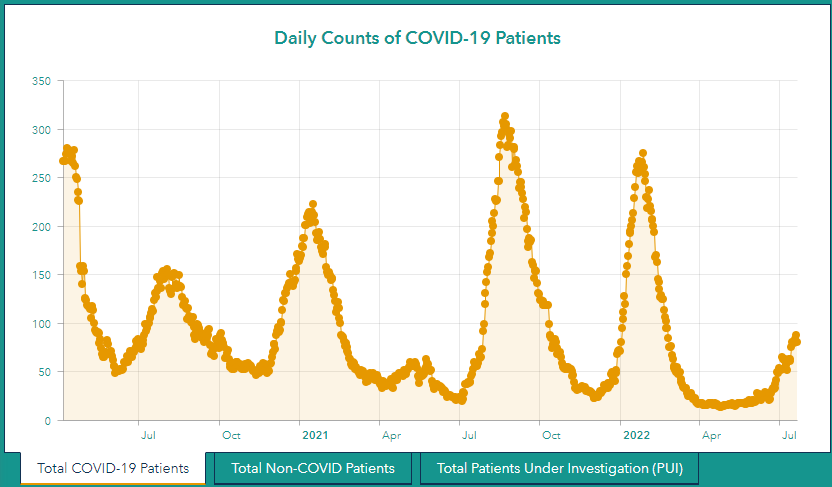
The table above shows you how multi-regional this increase is. But if we look at a graph of patient census, I actually think this is more impactful. First, here’s a look at the entire state’s patient census.
Then, let’s look again at hospital region K. Regions F, G, I, and L look similar.
When I see graphs like these, this is when I remember the scene from the movie, Jaws, when Martin Brody (played by Roy Scheider) says “we’re going to need a bigger boat.”
This week’s total cases are about the same as last week (+2%). Hospital admissions are about the same also (-2%). Deaths increased quite a bit, by 31%.
“Officials aren’t sounding the alarm”
In spite of all of this, I keep getting news alert headlines from national news media that the pandemic is not a big deal anymore. One great example even said, “Officials Aren’t Sounding the Alarm on Covid.” Maybe find some experts who haven’t given up on the American people and aren’t primarily motivated by midterm election results? I have plenty of peers who have been raising alarm for weeks.
However, I will say that my warnings are more muted than they have been in the past. I see the purpose of this newsletter to inform so that people know the risks and can make adjustments accordingly. But I’ve said from the outset that I’m not everyone’s mom and I can’t tell them what to do. Some days the two people who are my children don’t listen either. I’m reminded of the movie Don’t Look Up that came out last December. I found this movie hard to watch, especially the first time. At that moment, America was riding an Omicron-fueled rocket of suffering and death. The warnings and caution that so many of us were recommending felt unheeded, especially by our leaders. While the movie was about an asteroid heading to Earth, it paralleled really strongly with the global pandemic response and also efforts to combat global climate change. The main characters go on national television to warn the world. They can see what is coming. And no one takes them seriously.
At one point in the movie, the main characters take a more resigned perspective after exhausting all of their ideas. They go to the grocery store and behave as though everything is normal, even as there are signs everywhere that things are not okay. And I feel like this is sort of where some of us in public health are these days. We’ve been let down by our leaders, we don’t have the power or authority to influence change, and there’s not much we can do as individuals to quell this threat.
I don’t say this to complain. But if you’re seeing headlines saying that public health experts don’t think BA.5 isn’t a big deal, they’re asking the wrong experts and it may be because some public health experts are burned out and disillusioned. Today, I heard a colleague on public radio saying that as hospitalizations rise, we may need to put masks back on to care about others in our community. After months of our government and media coaching people not to care about our communities, but rather our economy, do we think that’s a switch that automatically flips back? The time to care about our communities is every day in big ways and in small ways. That lack of community care is part of what set us up to fail in our pandemic response. To be honest, it makes me seriously worry if anyone ever wanted to harm us on purpose. Our population would not mobilize to face the threat because we’ve been trained and encouraged to care mostly about ourselves.
In other news…
President Biden has COVID-19. I wish I could say that I’m surprised, but I’m not. The disease is everywhere, he’s flown internationally, and I don’t get the impression that he thinks this is a big deal anymore. His administration has minimized the threat for several months, and encouraged people to go back to work 5 days after testing positive, when people are still very infectious. [SIDE NOTE: he plans to ignore the CDC guidance that many of us has said is scientifically flawed and will isolate for the full 10 days]. If it is your perspective that the disease is not a big deal, you might take fewer precautions. Thankfully, he is fully up to date on vaccines. I hope he has a mild case and makes a full recovery. Here’s to everyone who has somehow outlasted Dr. Anthony Fauci and President Biden!
New York state records its first case of Polio in nearly a decade. I’ve often compared COVID-19 to polio - both cause mild disease in most people but survivors can have semi-permanent or permanent disability. Survival and death aren’t the only outcomes. And death isn’t the reason we vaccinate against polio - permanent disability is the reason we vaccinate. Thankfully, polio was eliminated in the US in 1979 due to widespread vaccination. But the anti-vaccine movement has been building steam for years and unfortunately this virus landed in the middle of a community that has historically been very opposed to vaccinations. Only 62% of the county’s 2-year-olds are up to date on their polio vaccine series, for example which is far below the state average and below what could be considered “herd immunity.” The disease spreads primarily through a fecal-oral route (you swallow someone else’s poop), which is why it was associated with swimming pools prior to vaccination. We are facing extreme heat throughout the US right now and pools offer welcome relief. Hopefully pool managers are monitoring chlorine levels. More broadly, I hope this illness can be contained, especially considering the community where it landed. Though, the US response to monkeypox does not give me a lot of reassurance that polio is under control.
Monkeypox is going ballistic, Mav! School starts very soon and the past two years of trying to advocate for COVID-19 preparedness in K-12 schools has taught me that no one is ready for what may be coming.
Despite what you may have heard, monkeypox is NOT a sexually transmitted disease. Nor is it limited to men who have sex with men. I think its explosion in the US and throughout the world is a coincidence of unfortunate timing during Pride Month. It is spread by close contact and sex is just one form of close contact. We have since seen monkeypox in children and the World Health Organization is warning that we should expect cases in children, pregnant women and the immunocompromised. Remember, the reason why K-12 schools and daycares require so many vaccinations is because there is a lot of enclosed spaces and densely populated rooms with close contact. The disease itself is pretty painful from the reports we’re seeing. It is now found in almost all 50 states.
There is a vaccine available for this, unlike for COVID-19 when it first arrived. The problem is that we don’t have enough for everyone. Meanwhile, cases are skyrocketing. The US response feels flatfooted and reminiscent of what we saw in March 2020. We need our leaders to take this far more seriously.
Unless otherwise stated, all data presented are publicly available from the Georgia Department of Public Health and the Georgia Geospatial Information Office. Graphs and images that were not produced by me are linked to the original source if you click on them. Thank you for your support of the COVID Digest.
My Ph.D. is in Medical Microbiology and Immunology and I am Chair of the Division of Natural Sciences and Mathematics at the University of Saint Mary. I've worked at places like Creighton University, the Centers for Disease Control & Prevention and Mercer University School of Medicine. All thoughts are my professional opinion, do not represent the views or opinions of my employer and should not be considered medical advice.










You are always brilliant, fusing scientific analysis with humane indignation toward our compassion-less capitalistic overlords. "Don't Look Up" is indeed a spot-on movie for our times!
Thank you!