Good evening readers! This may be a short newsletter (?), but I just wanted to provide some data and resources related to COVID-19 and the delta variant surge.
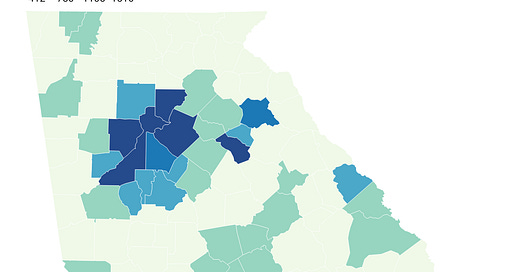
First, big thanks to Grant Blankenship of Georgia Public Broadcasting for sharing the results of an open records request from Georgia Department of Public Health (If any other journalists are feeling generous with their data, feel free to send them my way). The map below shows vaccination rates (1+ dose) for 12-15 year olds. When normalizing these vaccine numbers, there isn’t really a good census data set for the 12-15 year group. So I normalized against the county’s population. This map isn’t perfect, and it’s hard to say what is a “good” number at this point. What it really does is tell us which counties are doing better than others and which counties are most vulnerable. The data were current as of 05Jul2021. You can click on the map to see a live image where you can hover over a county of interest to see its number.
Nothing about this map should be surprising. It largely follows the trends on vaccination that we already have for adults. And that makes sense. Because if a county’s population of adults are declining vaccination, there’s little chance that they’re rushing out to vaccinate their teens. But one thing that sort of made me smile was seeing how many kids were vaccinated in different counties on the very first day of eligibility. This was one of those moments when you’re looking at data and feel a connection to the people they represent - because I vaccinated my son on the very first day he was eligible (his 12th birthday). These parents were not messing around.
As we think about who remains unvaccinated, one of the biggest demographic groups is children under the age of 12. There’s a misconception in the public that COVID-19 is harmless for kids. While it is often milder for children than for older adults, it does send kids to the hospital and they can die from it too. Just this week, a young boy from north Georgia passed away from COVID-19 disease. It is just breathtakingly sad and something we should prevent as much as possible. This week the American Academy of Pediatrics released a recommendation that everyone in a school setting over the age of 2 should wear masks, regardless of vaccination status, because so much of this population is not yet eligible to get the vaccine. For these kids, it’s as though they’re stuck in summer 2020, when vaccines weren’t available. Except that now the virus is spreading far faster and easier. And while a lot of people may have lost faith in the government throughout the pandemic, I would just like to point out that this is not a government organization saying this. It’s a group of 67,000 of America’s physicians who treat kids. Your child’s physician is likely a member. If you trust your child’s physician to mend a broken bone, we need to trust them on this too.
Speaking of vaccine data, DID YOU KNOW that Georgia DPH has expanded their data offerings to a census tract level? You can access this through their vaccine dashboard, but here’s a link to take you directly to it. There’s a lot of demographic data for sex, race, age and in combination.
The Advisory Committee on Immunization Practices is meeting on Thursday from 11:00 am to 4:00 pm eastern time to discuss some cases of Guillain-Barre Syndrome that occurred after receiving the Johnson and Johnson vaccine. You can see how the members weigh evidence and deliberate on the cost-benefit analysis. It’s all public and available via Zoom. The other thing they’re going to discuss is the potential for COVID-19 vaccine boosters for those who are immunocompromised. I won’t be able to watch the meeting live but you can access the meeting slides (when they’re uploaded), agenda and webcast here.
Things continue to intensify in Georgia. Here’s a look at test positivity for PCR and antigen testing.
The HHS Community Profile Report tells us how test positivity compares by age group. Any group above the red dotted line is one where we are missing cases. Note that test positivity is highest among kids aged 5-17 (K-12 aged children). This means that there is more disease among these children than we currently realize.
COVID-19 patient census is rising too. It’s rising in 12 of the 14 hospital regions across the state.
If we look at case rates over the past month, we can see that they are greatest in rural counties, but every county type in Georgia is rising. This is not just rural Georgia’s problem. Given time, we should anticipate that it will be every Georgia county’s problem. I would not assume that you’re in the clear if your county has 50% of its residents fully vaccinated. It just isn’t enough.
Of course, cases fuel hospitalizations and deaths, but it’s unclear how tightly they will be linked this time around since at least some of the state’s population is fully vaccinated. Consider this graph built using data from the United Kingdom. The third wave is the one they’re currently in. The second graph happened last summer, before vaccines were available. It’s a pretty compelling reason to get vaccinated as soon as you’re able to do so.
But if we look at what’s happening nationally in the US, it’s clear that this delta variant may have gained a foothold in Missouri and Arkansas, but cases are surging across large sections of the country. The graph below comes from the HHS Community Profile Report. It shows the percent change in case rate in the most recent week compared to the week prior. Anything in the mid-red color is at least a doubling of the previous week’s case rate. And there are a LOT of those counties.
And if we look at the bottom 20 states + territory for vaccination rate of total population, we can see that some of the states on this list are the counties being hit hard on the map above. The vaccines work really, really well. But they can’t save you from the worst outcomes of COVID-19 disease if you don’t use them.
Today I was invited to join Mitch and Autumn at the Good Faith Weekly podcast. I’m not sure how we found each other, but this was my third time on their show and some of the best conversations we have are the ones when we aren’t recording (figures!). Today they were telling me about when they interviewed John M. Barry, author of The Great Influenza, to gain any lessons learned or predictions for what could happen during the COVID-19 pandemic. And one of the things they asked Mr. Barry was why the American public took public health more seriously in 1918 compared to what happened with COVID-19. Mr. Barry suggested it might be because the symptoms were worse with the 1918 pandemic. But I’m not sure this is the whole story. Dying from COVID-19 is an ugly way to die, often accompanied by strangers. I don’t want to go into the details here, but it’s something I wouldn’t wish on my worst enemy. The difference is that last time a lot of people died at home or before they could get to a hospital. Their friends and family could see the worst that the disease had to offer and it took them quickly. With advances in healthcare, people with the most severe COVID-19 disease are treated in hospitals where their family has not been able to witness the horrors of the disease due to hospital policies (in place for good reason!). The people who bear witness to the ways that this virus destroys a body and takes a once healthy person to fighting for their life are our doctors, nurses, respiratory therapists, and others. The people who clean up the aftermath are the orderlies and custodians. I’m not arguing that more families should be allowed in the hospital or that patients should suffer at home - certainly not. But it’s an unfair burden we’ve placed on our healthcare workers while so many outside the hospital behave as though the devastation they see and feel is not real. Again, people don’t believe what they cannot see sometimes.
But we need to try. We need to do what we can to avoid hospitalization for COVID-19 in the first place. That includes getting vaccinated, yes. But with cases surging like they are and with the process to immunity taking 5-6 weeks, we need to bring in more of our non-pharmaceutical interventions like masking, social distancing, etc, as a stopgap. This isn’t for forever, but we need to do what we can to limit how bad this surge gets for our hospitals. Healthcare workers are leaving the field due to burnout and feelings that their communities have ignored them. How does that help any of us? Remember, there will be life and medical needs that have nothing to do with this pandemic. If you’ve seen how restaurant workers have left their industry due to the pandemic and perhaps you’ve been frustrated by service or how long it takes to get a table, imagine that same experience at your local hospital. I’ll leave you with this tweet from the President and CEO of CoxHealth, the hospital in Springfield, Missouri.




The COVID Digest is a free newsletter that depends on reader support. If you wish to subscribe please click the link below. There are free and paid options available.
My Ph.D. is in Medical Microbiology and Immunology and I am Chair of the Division of Natural Sciences and Mathematics at the University of Saint Mary. I've worked at places like Creighton University, the Centers for Disease Control & Prevention and Mercer University School of Medicine. All thoughts are my professional opinion, do not represent the views or opinions of my employer and should not be considered medical advice.