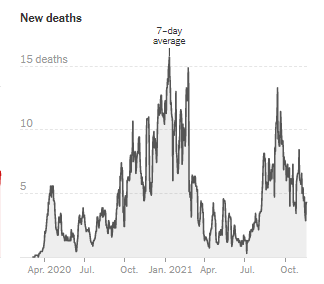
Unfortunately, the news is grim. The winter wave has begun for the United States. As far as cases go, it is most significant in the Midwest and the Northeast. I did a march through the data on Twitter earlier this week. But this week cases are inching up in Georgia too. And this week Georgia surpassed 30,000 COVID-19 deaths (confirmed + probable), a grim milestone indeed.
The national case graph is shown below from the New York Times COVID Tracker. It appears that cases are beginning to rise exponentially.
Yesterday, my undergraduate research student and I went on the University of Kansas Hospital System’s Morning Medical Update to share his recent findings regarding COVID-19 trends in the Kansas City Metro. He’s a senior biology major, about to graduate next month. He’s part of a class that we offer at the University of Saint Mary called Research Problems. Students pick a mentor to work with and identify a project that can be completed in a semester. He chose me and to work on COVID-19 data analysis trends. He did a great job yesterday and I was super proud of him.
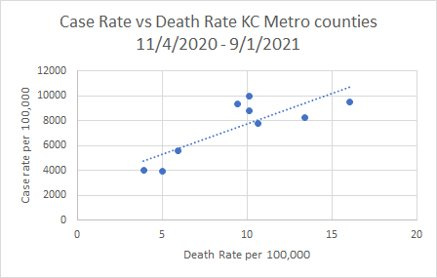
Briefly, he looked at the cumulative death rate per 100,000 for the nine counties that comprise the Kansas City Metro and compared that to the average for the region. We wanted to try to figure out why some counties were above or below the average in terms of successful strategies and/or lessons learned. He found that for counties that had no mask requirement at any time during the study period (04Nov2020 - 01Sep2021), the death rate was 24% higher than for counties that did. Additionally, we saw a 29% increase in death rate for counties that had no ICU beds compared to those that did have ICU beds. This makes sense since we know that accessing care fast is important for saving lives. But the biggest difference we found was based on vaccination rate. For the KC metro population that is aged 65+, the median vaccination rate was 75% as of 01Sep2021. Median is similar to average but different. It is the middle-most number in a range of numbers. For the total eligible population, the median vaccination rate was 43.1% as of 01Sep2021. For counties with a vaccination rate below the metro median, we saw a big increase in death rate. Considering vaccination rate for those 65+ (the folks most vulnerable to COVID-19 complications), the death rate rose 36% in counties that were below the median. For all those who were eligible for vaccination, the death rate rose 68% (!!) for counties that were below the metro median.
So clearly vaccines are important. But another wrinkle to this story is related to when were vaccines available and when deaths happened in Kansas City. Vaccines were first authorized in mid-December 2020 for healthcare workers and long term care facility residents. They didn’t become widely available in Kansas until April 2021. Meanwhile, the majority of Kansas City deaths happened during the winter surge of 2020-2021, so early in the study period.
So what the difference in death rates might mean when we consider counties above and below the median vaccination rate is a difference in collective safety culture among the population. At this late stage in the pandemic, seeing a county that still has a low vaccination rate might suggest an indifference toward recommended disease prevention strategies. And if that was the case by September 2021, then perhaps that same indifference existed with respect to mask wear, social distancing, etc, prior to the widespread availability of vaccines. In other words, the vaccination rate may be a proxy for general attitudes about safety surrounding the pandemic. A safety culture is often determined by the tone set by community leaders - mayors, county leaders, etc. So it is not surprising to me that we see low vaccination rates in counties that did not adopt a mask requirement.
The other thing we found was similar to what I have previously found for Georgia: the higher your case rate, the higher your death rate. There is a strong positive relationship between these two variables.
So if we want to prevent deaths, we need to prevent cases from happening in the first place. My student’s study indicated that vaccination rates, availability of ICU beds and mask requirements all made a difference with respect to death rates. A rural or outlying county can’t suddenly create ICU beds. So if you’re a leader in that position, you really need to consider bulking up the other two strategies (and others not studied here) including mask requirements, surge vaccination efforts, increase social distancing or consider a limit to indoor gatherings.
The rest of today’s newsletter will look at the trends in Georgia.
Keep reading with a 7-day free trial
Subscribe to The COVID Digest to keep reading this post and get 7 days of free access to the full post archives.