Dear readers,
We recently marked the three year anniversary of the first US cases of COVID-19. The COVID-19 pandemic severely impacted our lives through lockdown, quarantine, remote learning, infection, wearing masks and socially distancing ourselves, serious illness and - for far too many families - death. If we think back to February and March of 2020, I remember a lot of fear and a lot of unknowns. I remember seeing people who had the talent and skill and knowledge to lead us were not doing so. I had lost my mother in 2016. I hadn’t expected to be motherless at such a young age. And I wasn’t prepared to lose my dad too in the face of this new threat. This newsletter and the social media communication I was doing prior to its launch on Facebook and Twitter were born out of an intense need to know all that I could to protect my dad, to protect my children and husband, to protect my siblings and their children, and to protect myself. I had taught microbiology to nursing students who graduated into the front lines of the pandemic and I was in the midst of teaching first year medical students who didn’t realize that the world of medicine that they thought they knew was about to change in drastic ways. I didn’t have the training or skill to save lives through medical interventions like my students could. But I could try to keep as many people out of their hospitals as I could with good information. If I could protect my dad, perhaps I could protect others too.
I’m glad to say that Dad is fine. And so many of you are still here too, three years later. I remember hugging him for the first time since the pandemic started, in June 2021. He was full vaccinated (as were all of us) and he had survived unscathed. Victory! I had been able to coach him through disease prevention until vaccines became available and beyond.

I think the time has come to take a break from writing, at least about COVID-19. It used to be that I had an almost Pavlovian response to need to be at a computer at 4:00 pm EST every day because that’s when Georgia Department of Public Health would upload their data. That was early on in the pandemic. The cadence of data reporting has slowed to once per week and the timing has changed. Last week something weird happened - I forgot to go collect the data on Wednesday and didn’t think to do so until Friday. To me, this was the most in-my-face proof that I had truly burned myself out on COVID-19 and it was time to step away. The need to know and understand was always what drove me in this science communication effort. And I didn’t seem to need to know anymore. If the data didn’t motivate me anymore, then perhaps it was time to focus elsewhere.
Let’s go through the data we have to date on the pandemic for Georgia. Georgia is where I started this newsletter and its situation really isn’t all that different from other parts of the country at this time. First, let’s begin with cases. The graph below shows the weekly case total per week in Georgia since early on in the pandemic, 30Mar2020.
We can see the first summer surge, which seemed so massive at the time, peaking right over 30Jul2020. We can see the first winter surge followed by the advent of vaccines leading to steep declines in spring 2021. Then we see the Delta wave in summer 2021 followed by the biggest peak of all, Omicron, in December 2021. But we have seen two predicted surges since then. The summer surge of 2022 was about the same size as the summer surge of 2020. And the winter surge of 2022 - 2023 was the smallest one yet, even though historically the winter waves have always been so much worse.
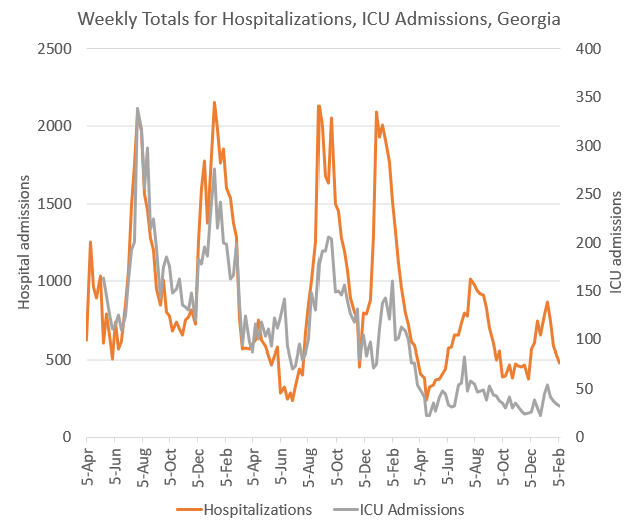
Of course, cases aren’t the most reliable indication of the intensity of the pandemic due to the wide range of severity for cases (from mild to severe), it looks like a lot of other things and so many people are taking home tests rather than the official ones that get counted by the states. For that reason, looking at the hospitalization data can be far more indicative of what’s going on. Below, you can see the graph for hospital admissions (orange line, goes with the left y-axis) and ICU admissions (gray line, goes with the right y-axis). These data, and all the others presented in this newsletter, come from the Georgia Department of Public Health.
What we can see is that the number of COVID-19-related hospitalizations reported each week has risen and fallen with each wave. For the first four waves, the peaks were about the same size. But after the Omicron wave in winter 2021-2022, the peaks became much smaller. In the most recent wave, fewer than 1000 Georgians were hospitalized for COVID-19 at the peak. When we look at ICU admissions we notice something interesting. With each successive wave, the peak for ICU admissions related to COVID-19 shrank. What could explain these two findings? My hypothesis is that after Omicron, infection was so widespread that nearly everyone in the country had been exposed to and developed some baseline of immunity to COVID-19 through infection or immunization. And while that immunity might not be bulletproof against every variant, it provided enough cross-protection that cases that came up after Omicron were milder than the ones prior to Omicron. In other words, far more of these were more manageable at home, rather than requiring a hospital bed or an ICU bed.
We can also look at deaths attributed to COVID-19 in Georgia. The graph below shows 5 major waves followed by two very small ones that are harder to define above the baseline.
Again, I think that a certain amount of cross-protection is conferred by vaccination and past infection, even if its not a perfect match for the variant circulating at the time. However, I would be reluctant to assume that this cross-protection lasts forever. The latest decision from the Food and Drug Administration is to administer the COVID-19 vaccine once per year, likely along side the flu shot. It will be designed and manufactured in much the same way as the flu shot in that they will have to predict months in advance (usually in the spring) the strains that will be circulating during the following winter. They can base this off of what is most common in the southern hemisphere (where it is fall and transitioning to winter). Sometimes their estimate is spot on, sometimes it is not. But even when it is not a perfect match, the flu shot often provides a lot of cross-protection and can reduce the severity of illness. That’s why I make sure my whole family gets it every year. We’ll be getting the COVID-19 vaccine, likely at the same appointment. In fact, the CDC has now added the COVID-19 series to the regular vaccines recommended for children (ages 6 months and up) and adults.
I plan to keep collecting data through 11Mar, because I want to have three complete years of case data. But this will be the final newsletter for the COVID Digest. I’m going to take at least a couple months off from this and then may consider relaunching the newsletter focused more broadly on science communication on a range of topics that are in the news. For paying subscribers, I’m pausing all billing during this hiatus. If and when I relaunch I’ll reach out to paying subscribers first so that they can make an informed decision in regards to continuing to support my work.
There is a sadness that comes with pausing writing right now. While I’ve never met many of my readers, some of you have shared such personal stories with me regarding your losses, worries, etc. Some asked for help better understanding the vaccines as they were pregnant and then sent me baby pictures after their beautiful children were delivered. I have made valuable friends through this work - in politics, in the news media, in civic organizations, and in public health and government.
But there is also joy in recognizing that the reason I can pause writing right now is because the pandemic is in a much better place than it was three years ago. Like many other scientists around the country, I stepped up to the microphone to explain what was happening to try to educate those around me so that they could make informed choices about preventing disease. I’m grateful to have been born in the time and place that I was so that I could have the opportunities and education to serve my dad, my family and all of you in this way. I’m proud of this work. I’m pleased to say that a lot of people know more about how disease spreads and how to access and understand data. Hopefully this will prepare people to have more confidence if and when we are faced with a similar crisis.
I wouldn’t say that the pandemic is over. And my heart goes out to those who are immunocompromised and having to navigate a treacherous disease landscape. As the public health emergency lifts, I think we will see disparities in health that are already all too familiar in this country. We must do more to make sure that those who have been medically underserved continue to have access to health education, routine and preventative care, robust availability of nutritious food, mental health, vaccines and other tools that are important in preserving both quantity and quality of life. I want to applaud and support those who work tirelessly in public health and public health policy who have been working these issues for years and who will continue to do so in the years to come.
With the utmost gratitude for your readership, trust and support, I am signing off now for the COVID Digest.
Amber Schmidtke, Ph.D.
My Ph.D. is in Medical Microbiology and Immunology and I am Chair of the Division of Natural Sciences and Mathematics at the University of Saint Mary. I've worked at places like Creighton University, the Centers for Disease Control & Prevention and Mercer University School of Medicine. All thoughts are my professional opinion, do not represent the views or opinions of my employer and should not be considered medical advice.





I have a lot of empathy for your burnout. But I won't lie, it feels like you're one more person deserting those of us who are immune-compromised and trying to navigate a world that has given up trying to provide information or protection. This is very frustrating, since you are one of only 3 remaining sources of information on COVID-19 who are taking it seriously in any way. I don't mean to put this directly on you-- there should be an entire public health response and the CDC and other public health officials are simply abdicating their responsibility here-- but it feels like the walls are closing in as more and more folks just throw in the towel and resign themselves to THIS state of affairs. Deaths are still high. Long Covid is still a huge problem that vaccination doesn't prevent.
Those of us who still have to care about COVID to survive and don't have the luxury of throwing our hands up? We're being left out in the cold. It's incredibly difficult not to feel bitter and angry and hopeless.
Thank you so very much for being one of the voices of reason for the past few years. I have really appreciated your ability to share the data and point out what it means as well as what the uncertainties are.