Hello readers! In case you’ve missed it, there is a lot of disease going around right now for COVID-19. I know several people who have fallen ill this week, including at least one friend who was extremely careful. Thankfully all of these folks are vaccinated and experiencing mild symptoms, but it would be naive to assume that there is no risk in going to public places unmasked these days.
For example, let’s look at the map below that comes from the CDC. The map is linked to the website, but you may need to click on “Community Transmission Levels” to see this particular map. I think the default setting is to show you Community Levels (I’ll explain the difference in a second).
The map above can be thought of as the risk that you will be exposed to COVID-19 in your county if you’re in a high risk situation (indoors, crowded, poor ventilation, etc). You can see that about 95% of US counties are in the high or substantial risk category for exposure. The map is built on recent case rate and recent test positivity. However, because testing is not as available as it used to be and many prefer to test at home (which goes unreported), this map represents the best case scenario. The reality is likely worse than what we see here, and especially for the South. That’s because if we look at test positivity by region, we can see that things are really spiraling out of control in the South (green). There is nowhere near enough testing to identify the amount of disease that is out there. This graph comes from the HHS Community Profile Report.
The Community Levels map (shown below) can be thought of as the risk that you would have a hard time accessing a hospital bed if you needed one. This is based on recent case rate, COVID-19 patient census and new COVID-19 hospital admissions. If you’re in the high (orange) category, the CDC has suggested that individuals resume masking or other efforts at disease control. You may notice that 19.5% of US counties (including some that have high population density) fall into this category. The number of counties that are in this category is also growing each week.
This matters because some will say that given a high vaccination rate in some parts of the country the cases aren’t as important as the hospital burden. This attitude is a declaration that leaders have given up on disease control and it might make sense initially until you remember that people don’t end up in a hospital without getting sick in the first place. If you want to drive down COVID-19 hospital admissions, you need to drive down infection in the first place. The idea of “don’t worry about cases” sort of shifts the burden to healthcare workers to manage an ever-growing patient census, so that life can continue as “normal” outside the hospital walls. Relying on hospital admissions going down when the virus runs out of people to infect means sacrificing a lot of your people in the form of their lives, semi- to long term disability (Long COVID), or missing time from work and daily life because one is out sick. Instead, we’re expected to manage the biggest group project ever as a collection of uncoordinated individuals.
The state of Georgia is our focus for today and they update their dashboards on Wednesdays. There are a few highlights I want to address and then dig deeper.
Cases are down slightly (by 5%), but I think this is an artifact of 4th of July closures for testing centers and healthcare facilities where people get tested. I would not be surprised if we have a big case week next Wednesday as the backlog of delayed tests is cleared. I would hypothesize that this week’s case total is as large or larger than the previous week (~20,000 cases reported per week).
Hospitalizations are up this week by 12% and ICU admissions for COVID-19 are up by 4%. More concerning to me, however, is that patient census is rising quickly for multiple hospital regions. This metric shouldn’t be impacted by 4th of July closures. When they start turning sharply upward and doing so together, that’s historically been the warning that something big is coming.
Deaths are down this week by 30%. This may also be impacted by the 4th of July holiday, but I don’t think that explains all 30%. The other thing to note is that Georgia recorded another pediatric death this week, the 38th COVID-associated death since the pandemic began.
Cases
Let’s start with a look at where recent case rate (cases per 100,000 residents) is most intense in Georgia. The more orange or red a county is, the more intense it is. You’ll notice there are very few counties in the pale yellow category anymore. There are a growing number of orange and red counties, many of which are clustered in the southwest corner of the state (hospital regions I and K).
We can also look at who is getting sick. The graph below shows the weekly case totals per age group over the past 8 weeks so that we can compare age groups and see trends over time.
A few things stand out to me: (1) even with the 4th of July testing and reporting delays we can see that cases continue to rise for children under 5 years old (only recently became eligible for vaccinations) and those 80+. Remember, because of the reporting delays, this case total represents the best case scenario. (2) We missed at least one day’s worth of testing, possibly more this week if testing centers closed for the whole holiday weekend, as an example. Cases appear to be lower for those 18 - 69, but I suspect this isn’t reflective of reality due to the holiday. Problem is that I can’t tell you how “off” these totals are. We’ll just have to wait until next week to find out. (3) K-12 aged children are the only group to see flat cases over the past 8 weeks despite what’s happening with all the age groups around them (i.e. parents, grandparents, etc). I don’t know that this means they aren’t getting sick; it may be that we’re not looking for disease in these age groups now that school is out for the summer.
Hospitalizations
The graph below shows the weekly totals for COVID-19 admissions to the hospital (orange) and ICU (gray) in Georgia. You can see that hospital admissions have been rising sharply, by 200%, since late April.
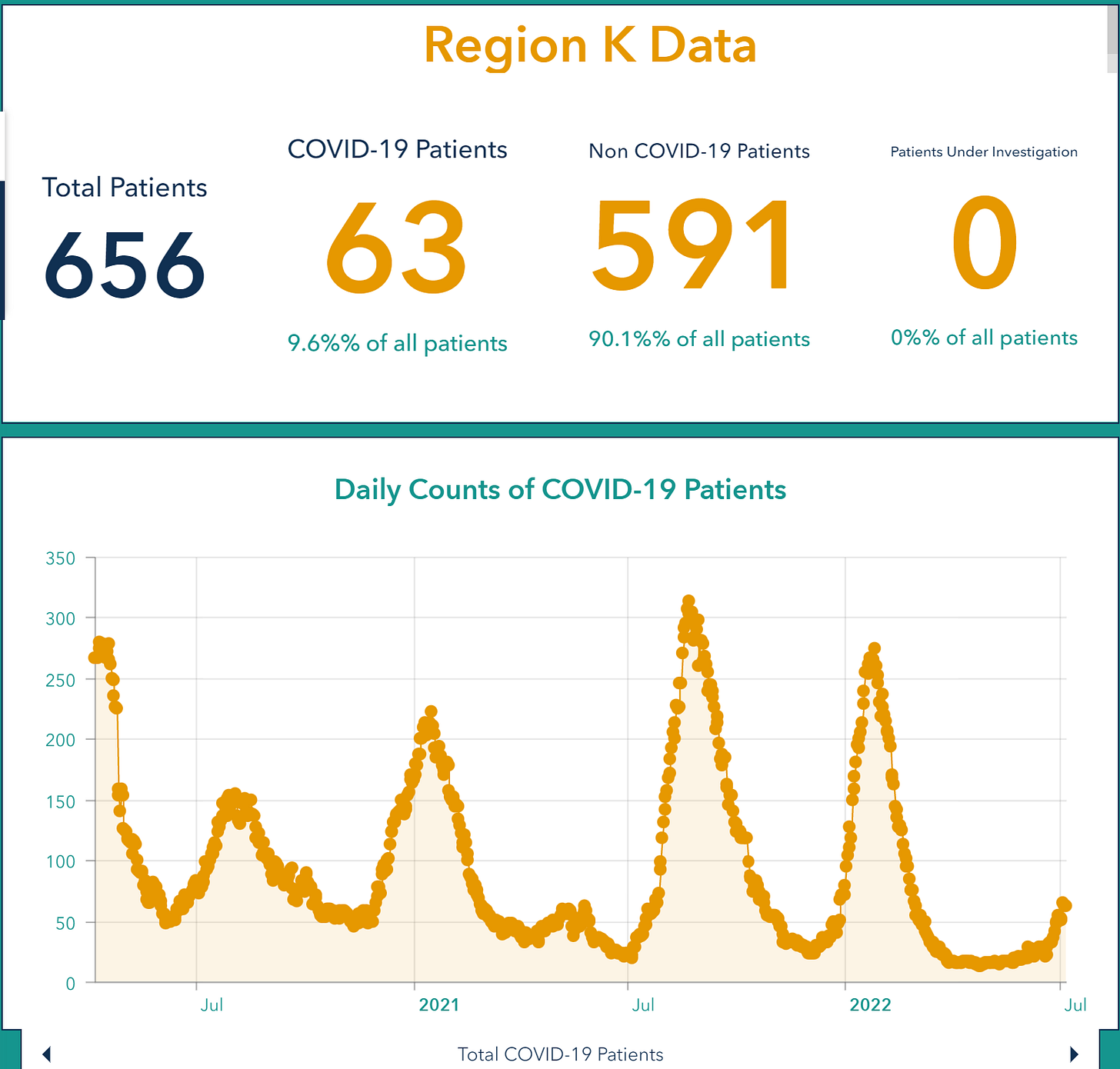
However, to me, the bigger worry is what’s happening with patient census, or how many people are currently in the hospital with COVID-19. This is how we’ve been able to best see how good/bad things are in the past. As of today’s update, there are 1134 patients currently in the hospital for COVID-19 in Georgia. Compare that to 348 on April 20 (the same time frame that I compared for hospital admissions). You can explore patient census using the Georgia Geospatial Information Office Data Hub. Last week there was one hospital region that had transitioned from the green to yellow zone (stop light color coding where red is most intense and green is least intense). This week there are now 4 regions in the yellow zone: A, B, K and N. When you look closer at each region, there are multiple regions that are seeing a sharp increase over the past week or two. Region K (southwest Georgia) is shown below, but similar trends are observed for regions A, B, G, and I.
For reference, I’ve provided the map below that shows how the Georgia hospital regions are divided.
The patient census data for the Georgia hospital regions doesn’t often agree. The one time when there seems to be solid agreement is when surges begin. To me, having watched the data on this pandemic for Georgia since the beginning, seeing multiple regions all trend sharply upward at the same time is a bad sign.
I think things are about to intensify for Georgia, based on what the hospital census data are showing us.
Unless otherwise stated, all data presented are publicly available from the Georgia Department of Public Health and the Georgia Geospatial Information Office. Thank you for your support of the COVID Digest.
My Ph.D. is in Medical Microbiology and Immunology and I am Chair of the Division of Natural Sciences and Mathematics at the University of Saint Mary. I've worked at places like Creighton University, the Centers for Disease Control & Prevention and Mercer University School of Medicine. All thoughts are my professional opinion, do not represent the views or opinions of my employer and should not be considered medical advice.