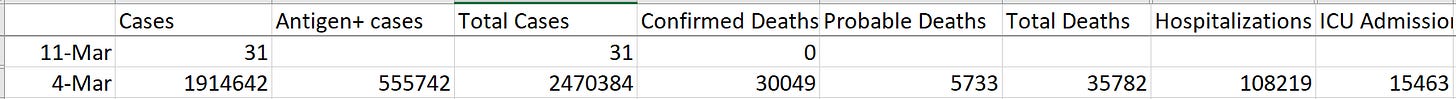
Good morning readers! As we start the month of March, we are approaching the 2 year anniversary of when COVID-19 really changed our lives. We are coming up on the first day that I started collecting data from the Georgia Department of Public Health and sharing what I knew about data, trends and how diseases typically work to family and friends who were scared and didn’t know what to do. I looked back and we can see the heavy toll of 2 years of disease.
In two years, we’ve seen 2.47 million cases between PCR and antigen testing. There have been 108,219 hospitalizations and 15,463 ICU admissions. We don’t have data on how many people survived the infection but suffer from Long COVID. But we do know that at least 30,049 confirmed COVID-19 deaths have been recorded and an additional 5733 deaths are likely linked to COVID-19. For Georgia, this is the equivalent of losing the entire city of LaGrange, Lawrenceville or McDonough.
Nearly two years ago I was asked to give a briefing on COVID-19, what we knew and what we didn’t know, to my medical student group at Mercer University School of Medicine. They were scared for themselves, their parents and grandparents, etc. About a week later that briefing became a full presentation to the entire campus community. This week, I was asked by my current university to recommend new community transmission thresholds at which I would be comfortable making masks optional. I think many people see through the purely political adjustment of community transmission thresholds that CDC has set and want to see what they should do instead. So I thought that if I was giving this advice to one organization, I should offer it to my readers too.
Remember that with this disease we want to think of disease prevention like stacking pieces of swiss cheese. As you may know, swiss cheese has holes in it, which works with disease prevention of COVID-19 because none of our strategies are 100% effective. However, if we layer enough pieces of cheese together, it is more likely that we overlap them in such a way that there are no holes from one side of the stack of cheese to the other. The graphic below comes from the New York Times.
Ideally, we want to layer 2-3 strategies together at all times. Being vaccinated and boosted counts as one strategies. If case rates are low, that’s another one. Open a window and you’re good to go. However, if case rates are NOT low, then that strategy is no longer serving us. We need to add another strategy to take low case rate’s place. So the next thing to consider is masks. For this reason, things like case rates and test positivity can still be really helpful in determining whether masks are needed.
If you recall from last week’s email, the new CDC transmission levels took all of the previous thresholds and redefined them as “low” community transmission, with a ceiling of 200 cases per 100,000 over the past 7 days. That seems kind of ridiculous. In addition, this week we learned that vaccine efficacy for 5-11 year olds does not seem to be as robust as what is observed for 12-17 year olds, likely because they receive a lower dose. That might explain why so many of our fully vaccinated kids got sick during the Omicron wave. So waiting to mask until you reach 200 cases per 100,000 in a community means you’ve already put a lot of people, including children, pregnant people and those who are immunocompromised at heightened risk.
Keep reading with a 7-day free trial
Subscribe to The COVID Digest to keep reading this post and get 7 days of free access to the full post archives.